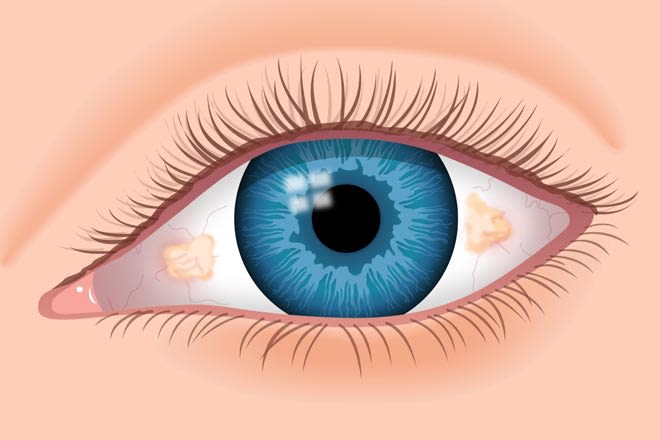
What is conjunctivochalasis?
Conjunctivochalasis (CCh) is a condition in which the clear outer layer that covers the white part of the eye (the conjunctiva) loosens, creating wrinkles and folds. This can cause a range of symptoms that include discomfort, dry eyes and blurred vision. It is most commonly found in older populations. CCh is often bilateral — affecting both eyes.
CCh was first described in 1908 by Anton Elschnig. In 1942, Wendell Hughes named the condition using the Greek word chalasis, which means “to slacken.”
What causes conjunctivochalasis?
The cause of conjunctivochalasis is not yet fully understood.
Many parts of the body, like the lungs, bladder and skin, have a certain level of elasticity. This allows them to return to their original shape after being stretched (like a rubber band). As a person ages, these tissues lose some of that elasticity. CCh may be a sign that the tissue of the eye has lost its ability to go back to its original shape after being stretched.
When the eyelids open and shut, they rub against the conjunctiva, causing friction. This may cause the elastic fibers in the outer layer of the eye to break down. This may then lead the conjunctiva to develop folds that run parallel to the eyelids. These folds are a characteristic trait of CCh.
Other theories about the cause of CCh include:
- Eye rubbing
- Eyelid position abnormalities
- Ocular irritation
What are the signs and symptoms of conjunctivochalasis?
Some individuals with conjunctivochalasis may not experience any symptoms. For those who do experience symptoms, they can be mild to severe.
Signs associated with CCh may be a “glazed” or jelly-like appearance of the white part of the eye. Two other conditions, conjunctival chemosis and allergic conjunctivitis can appear the same. Allergic conjunctivitis is usually accompanied by itching of both the eyes and the nose as well as sneezing. Chemosis presents with more swelling and can be caused by allergies, eye surgery, exophthalmos (bulging eyes) and lagophthalmos (inability to close the eyelids).
Dry eyes
Conjunctivochalasis is sometimes confused for dry eye syndrome. However, the presence of loosened conjunctiva can help distinguish between the two. Individuals with CCh may also notice that discomfort increases with frequent blinking. This is likely due to the inability of the upper eyelid to reach the tear meniscus.
The tear meniscus, or tear lake, is a strip of tears along the bottom eyelid. Normally, when an individual blinks, the upper eyelid dips into this strip of tears to help lubricate the surface of the eye. When it is unable to do so, it can lead to dry eye and discomfort. The conjunctival folds associated with CCh can interfere with and even destroy the eye’s tear meniscus.
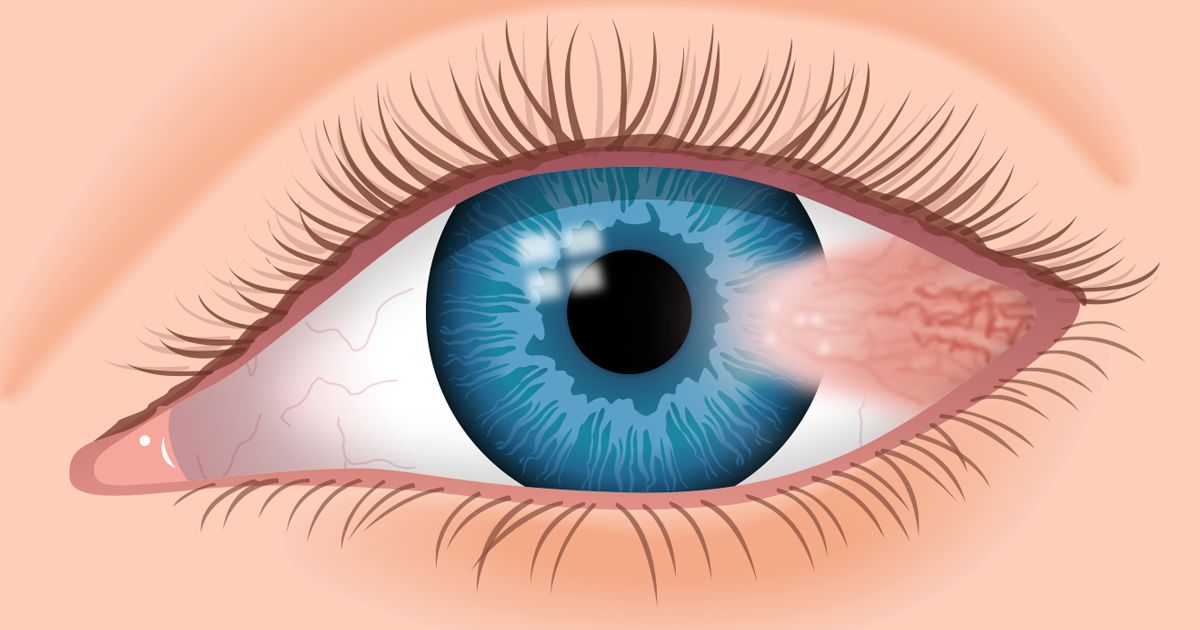
Epiphora
Epiphora, an abnormal overflow of tears onto the face, is a potential symptom of conjunctivochalasis. Epiphora can be caused by excessive tear production or lack of effective tear drainage. For those with CCh, the conjunctival folds may block the puncta, the tear ducts that allow for drainage.
This effect is common in individuals with conjunctival folds nearer to the nose. It can also worsen when the affected individual looks in the direction of their tear ducts.
Exposure keratopathy
One of the more severe symptoms of conjunctivochalasis is exposure keratopathy. This is a condition that occurs when dryness damages the cornea. The cornea is a clear layer that covers the iris and pupil, and allows light to enter the eye. Exposure keratopathy is triggered when the eyelids are unable to close all the way.
If left untreated, exposure keratopathy can lead to permanent vision loss.
Other symptoms associated with conjunctivochalasis are:
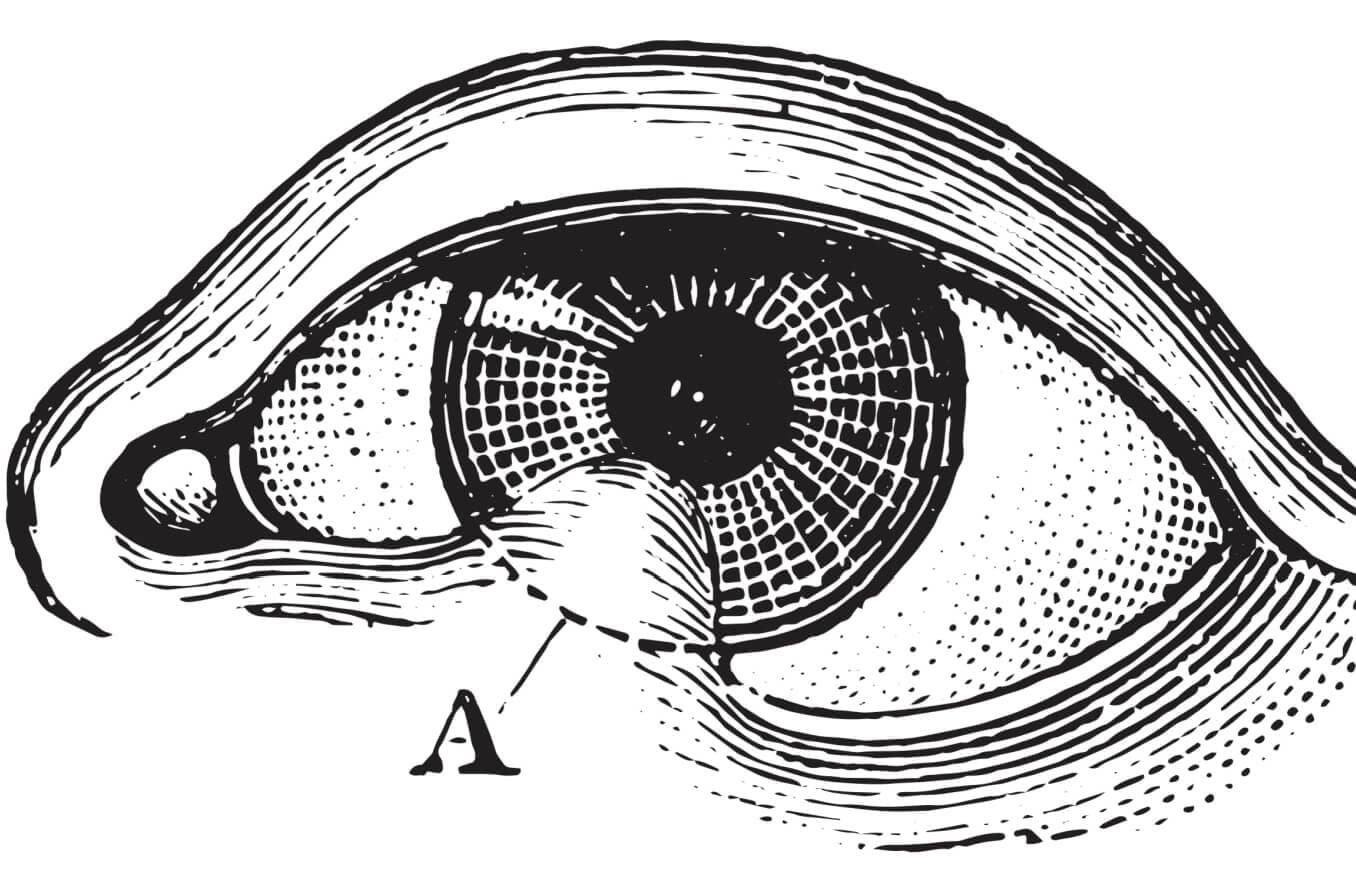
How is conjunctivochalasis diagnosed?
Conjunctivochalasis can be difficult to diagnose and is often misdiagnosed as dry eyes or allergies. If an eye doctor suspects CCh, they will likely perform a slit-lamp examination. A slit lamp is a microscope with a bright light that allows the doctor to see the layers of the eye more clearly.
If a patient has CCh, the doctor will likely find:
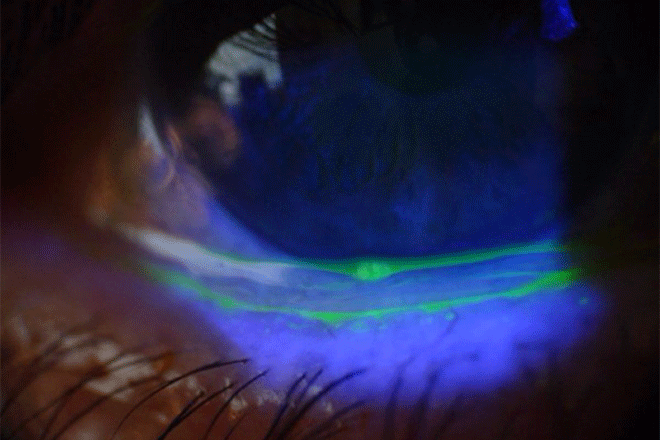
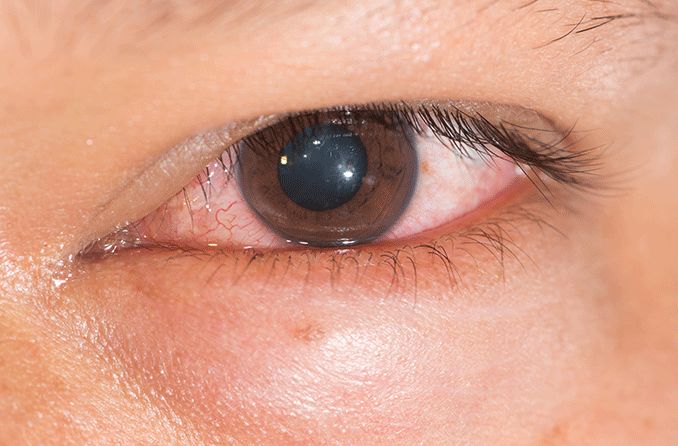
Image of eye stained to detect conjunctivochalasis. [Image credit: Conjunctivochalasis by Lindendoss is licensed under CC SA 1.0]
- Loosened and folded conjunctiva
- Blocked or destroyed tear meniscus
- Dry eyes
- Blocked tear drainage with epiphora
- Inflammation on the eyelid
- Fluorescein, lissamine green or rose bengal dye will stain the conjunctiva and make the folds more visible
One way to find the cause of folds in the conjunctiva is to use allergy drops or redness removing drops. Allergic conjunctivitis will improve after using the drops while CCh will not.
Physicians frequently use a grading system to label the severity of CCh. Hoh et al.’s system is based on the number and height of the conjunctival folds:
- Grade 0 (no persistent fold)
- Grade 1 (a single small fold)
- Grade 2 (two or more folds but not higher than the tear meniscus)
- Grade 3 (multiple folds and higher than the tear meniscus)
Other grading systems include further details, such as:
- Where the folds are located on the eye
- How high the folds are
- Whether or not the tear ducts are blocked
- How quickly the folds move back into position after blinking
- If the effects change when the patient looks down or rubs their eyes
How is conjunctivochalasis treated?
Treatment for conjunctivochalasis is based on the severity of the condition. If a patient is asymptomatic, no treatment is needed. For mild cases, the approach will likely focus on treating symptoms rather than the CCh. Artificial tears and allergy eye drops can help with dry eyes and inflammation.
In more severe cases, the patient may undergo surgery to remove part of the conjunctiva. The remaining conjunctiva is then closed, either with a small stitch or surgical glue.
Another option for CCh treatment is thermal cautery. Thermal cautery involves the use of heat to destroy a small amount of tissue. For those with CCh, this procedure can cause the conjunctiva to contract, which can then help restore the outflow of tears.
When should you see a doctor?
If you notice consistent eye dryness, burning, discharge or an overflow of tears, or if the white part of your eyes looks swollen, it is important to seek attention from an eye doctor. If these issues worsen when you look down, blink rapidly or rub your eyes, this may be an indication that you have conjunctivochalasis.
Conjunctivochalasis is frequently misdiagnosed or missed altogether. It is important to have a coordinated health care team to help with proper diagnosis and treatment.