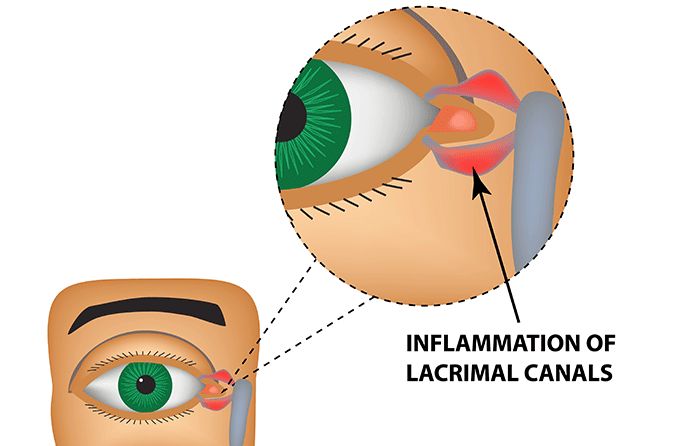
What is canaliculitis?
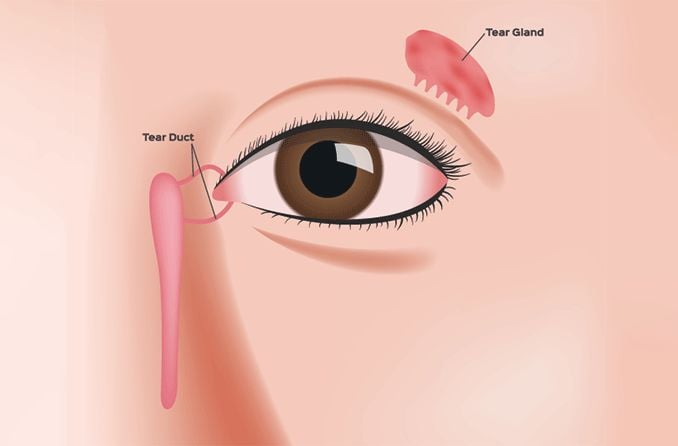
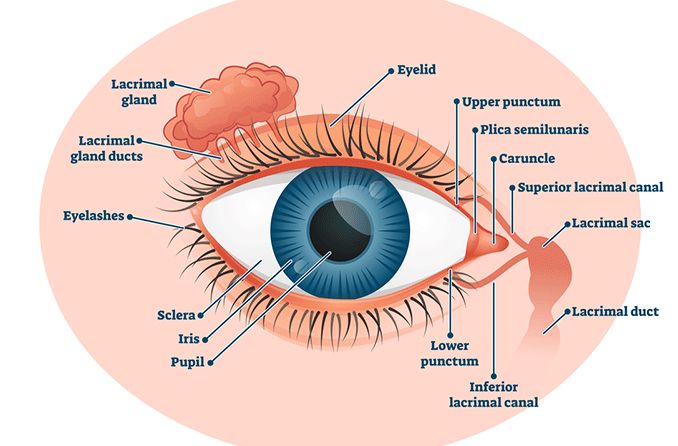
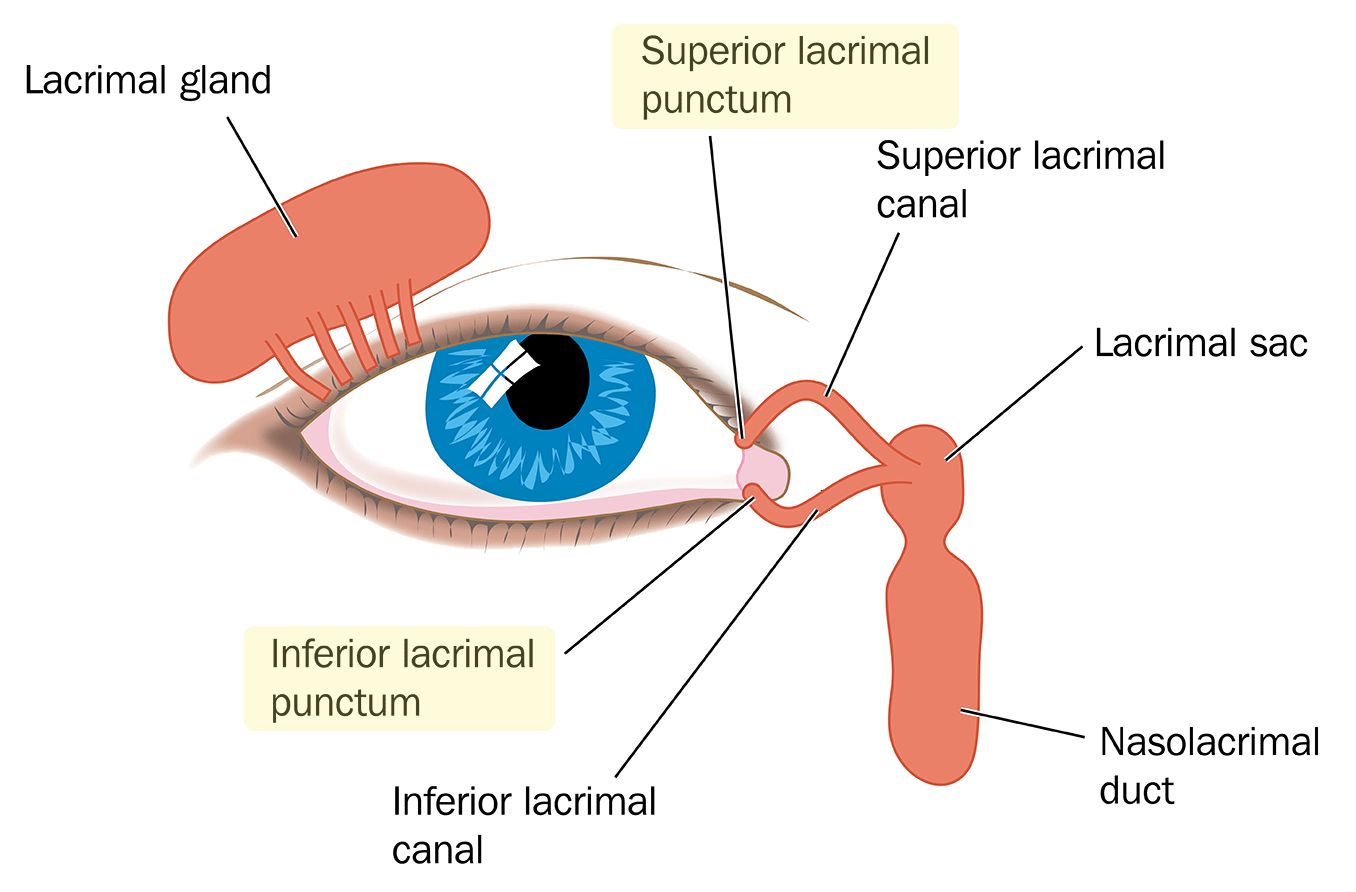
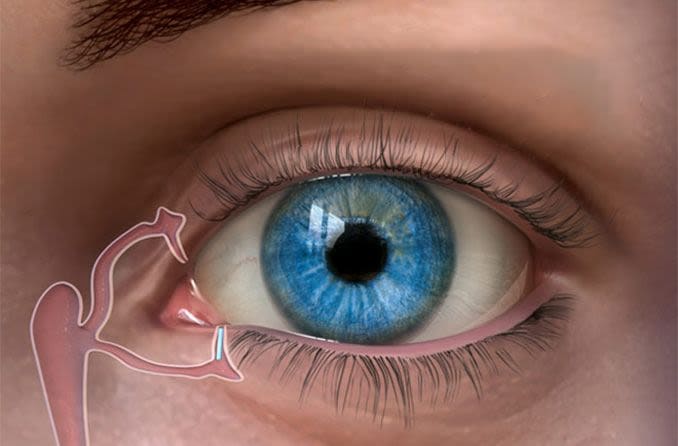
Canaliculitis is an inflammation or infection of the tear duct or canal (the lacrimal canaliculus). It is a relatively uncommon disease with symptoms such as tearing, discharge and swelling in the tear duct opening. Because of its rarity and common symptoms, canaliculitis is frequently misdiagnosed.
It’s often unilateral, which means it only affects one eye. So, it is unlikely that someone would have canaliculitis in both eyes at the same time.
Canaliculitis makes up only about 2% to 4% of lacrimal (tear-related) disease cases. It’s more common in females than males and has been shown to occur in people ranging in age from 5 to 90. The average age of patients, however, is around 65.
What causes canaliculitis?
Canaliculitis is caused by an infection of the lacrimal canaliculus, the tear ducts and canals. This infection is usually the result of bacteria, but fungi and viruses have been known to cause it as well.
The most common cause of secondary canaliculitis is punctal plugs, which are often used as treatment for dry eye. One study found a 6% rate of canaliculitis occurring in patients who received SMARTPlugs. However, the actual rate may have been even higher since a number of patients did not return for follow-up visits in the years following plug insertion. The average time between plug insertion and canaliculitis symptom development is around three years.
A possible reason that canaliculitis is seen more often in women than men is the hormonal shift undergone during menopause. This shift can lead to decreased tear production that results in lower protection against infection in the eyes.
There’s another theory that the use of eye makeup may increase infection risk, as it can obstruct the tear duct and introduce bacteria, leading to increased bacteria production.
Symptoms of canaliculitis
Canaliculitis has a variety of symptoms that vary from person to person. The most common symptoms are:
Discharge from the affected area
Other symptoms of canaliculitis include:
Concretions (small white or yellowish spots on the eye)
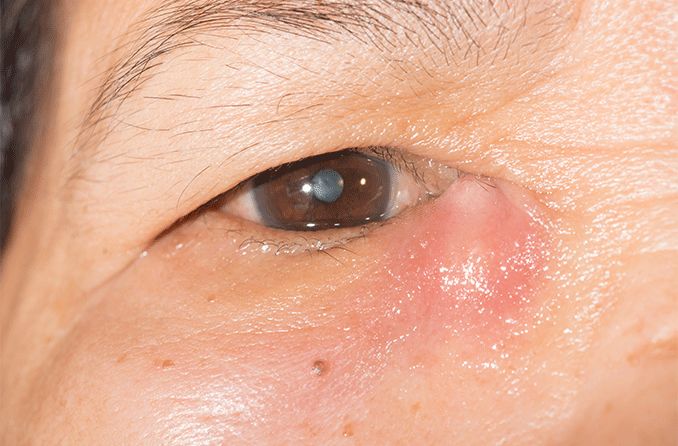
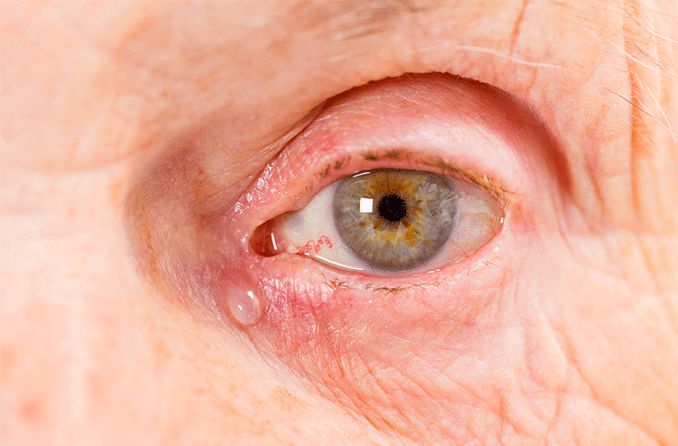
Swelling in the corner of the eye
Erythema (reddened skin)
Swollen, red punctum — the small opening in the corner of the eye through which tears drain — that is pushed outward (called a pouting punctum)
Irritation
Feeling that something is in your eye (foreign body sensation)
Symptoms that may occur as a result of secondary infection by punctal plugs include:
Bloody tearing
Blood-tinged discharge
Protrusion from punctum
How is canaliculitis diagnosed?
Due to its rarity and variety of symptoms, canaliculitis is frequently misdiagnosed, most commonly as:
Chronic conjunctivitis – This is chronic inflammation of the clear membrane that covers the sclera (the white of the eye) and the inner eyelids. Common symptoms include redness, irritation, burning and discharge.
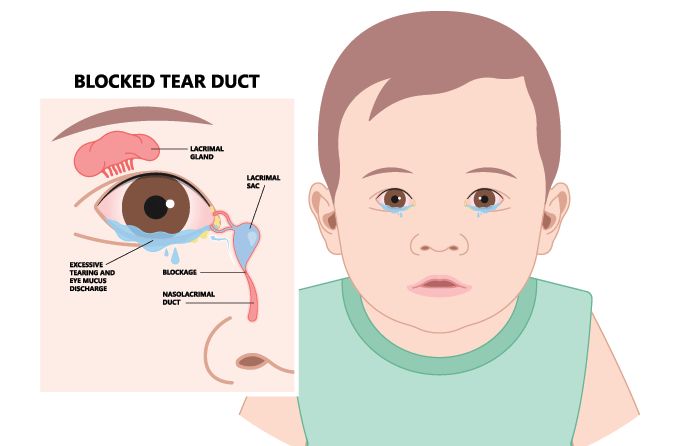
Dacryocystitis – This is an infection of the lacrimal sac. Common symptoms include pain and swelling in the corner of the eye near the nose, redness, tearing, discharge and/or fever.
Migrated punctal plug – This is uncommon, but can occur if a punctal plug moves deeper into the lacrimal canals. Common symptoms include pain and excessive tearing.
Carcinoma of the lacrimal canaliculus (an extremely rare form of cancer) – Common symptoms include excessive tearing, bloody discharge, bloody nose and the presence of a mass.
Because misdiagnosis happens so often, it is not uncommon for the disease to go years without proper treatment. If you suspect you might have canaliculitis, however, a review of your symptoms and a clinical examination by an eye doctor can lead to a correct diagnosis.
Your eye doctor may order additional tests to diagnose your condition, including:
Microbiological culture examination – This exam allows your eye doctor to determine what microorganism is causing your infection.
Histopathological examination – For this exam, a tissue sample is taken and studied to determine the extent of a disease’s symptoms in the patient.
Ultrasound biomicroscopy (UBM) – A UBM is a noninvasive imaging test that can provide detailed information on the eye’s condition.
Dacryoendoscopy – This is an examination of the canaliculi and tear ducts with a light and camera attached to a flexible tube.
Dacryocystography – In this imaging technique, liquid is injected into the lacrimal system and used to find obstructions.
Canaliculitis vs. dacryocystitis
Due to their similarities, canaliculitis is sometimes misdiagnosed as dacryocystitis. Where canaliculitis is inflammation of the tear duct, dacryocystitis is caused by an infection of the tear sac (also called the lacrimal sac). Only an eye doctor can diagnose which condition you have.
Your eye doctor will be able to determine what condition you have after a comprehensive eye exam. Typically, if the corner of your eye becomes red and puffy, it is more likely to be canaliculitis. If the swelling is just under the corner of your eye, above where the tear sac is located, it is more likely to be dacryocystitis.
How is canaliculitis treated?
Non-surgical treatments exist for canaliculitis, but usually aren’t enough to get rid of the infection entirely. Surgery followed by medication is thought to be the most effective method of treatment.
First-step treatments include:
Topical antibiotics
Antibiotic irrigation
Warm compresses
Removal of infected material
These treatments are not one-time cures, and the infection often reappears again later. However, there are cases where these treatments may eventually resolve the condition completely.
If non-surgical treatments are unsuccessful, an operation called a canaliculotomy may be necessary to open up the blocked duct and canal.
In cases where canaliculitis is caused by a punctal plug, removal of the plug(s) will often resolve the issue. Canaliculitis caused by punctal plugs also has a lower chance of recurrence in patients.
When to see a doctor
If you experience any eye pain or discomfort for a prolonged period of time, you should schedule an appointment with your eye doctor. A thorough evaluation of symptoms and a comprehensive eye exam can lead to proper diagnosis and treatment.
It is also important to see your eye doctor for a follow-up assessment if you had punctal plugs inserted in the past three to five years.
READ NEXT: What is dacryoadenitis?