Periorbital cellulitis is an infection of the eyelid or of the skin around the eye. It most commonly affects children under five years of age, though sometimes adults can suffer from it as well. Symptoms include redness, tenderness and swelling around the eye. The condition needs to be diagnosed and treated promptly by a doctor to make sure it is not a different and more serious condition, orbital cellulitis, and to prevent any complications. Periorbital cellulitis is not contagious.
Periorbital cellulitis symptoms
Both children and adults have similar symptoms, although children’s symptoms can be more dramatic and a bit more severe. The symptoms occur around one eye only. Here are some typical symptoms of periorbital cellulitis:
Pain and tenderness in or around the eye.
Swelling of the eyelid and the soft tissue surrounding the eye.
Soreness and tenderness in the nose area.
Redness and irritation around the eye and on the white of the eye.
A break in the skin through a cut, scratch or perhaps an insect bite near the eye.
Possibly a small bump on the eyelid called a stye or chalazion.
A fever (a temperature over 100 degrees).
A study published by the American Academy of Ophthalmology found that children under five were more likely to have had a localized infection (such as pink eye) before coming down with periorbital cellulitis. Older children were more likely to have had a cut, scratch or other injury prior to showing symptoms.
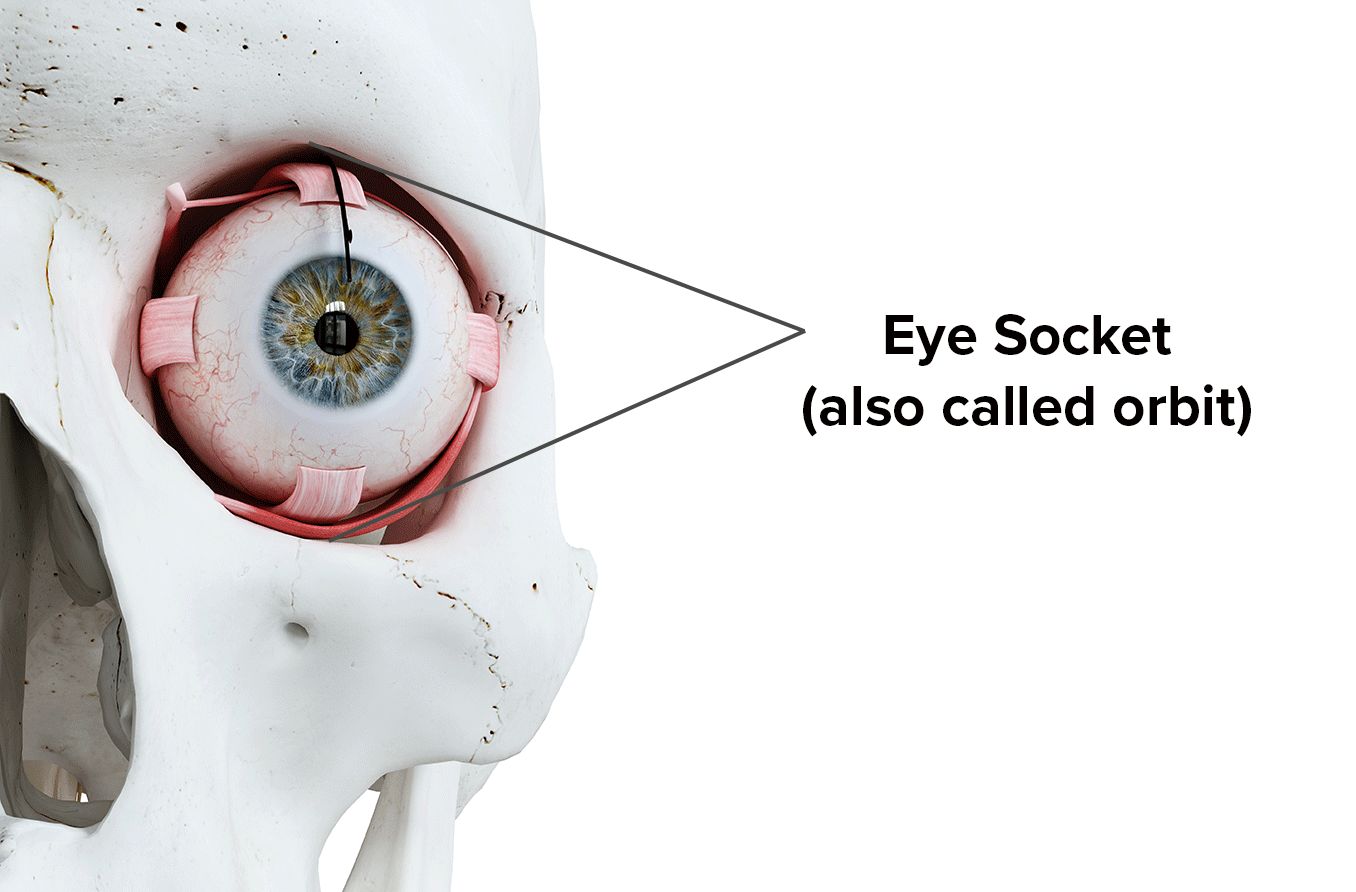
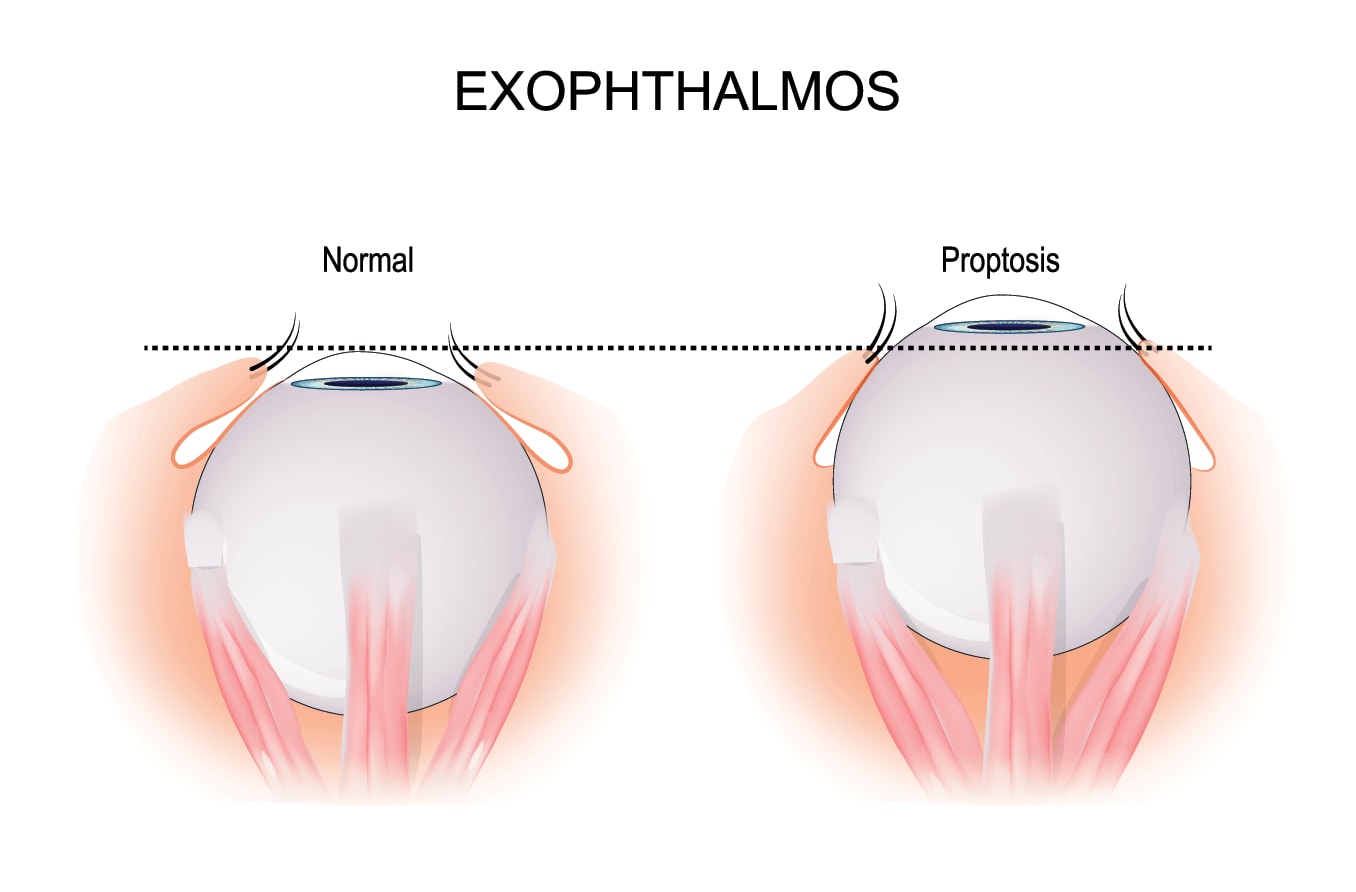
There is no pain with actual movement of the eye, and vision is normal. The infection in periorbital cellulitis does not spread into the eye itself, because the eye is protected by a layer of tissue called the septum, which separates the front part of the eye from the back part of the eye.
Periorbital cellulitis, however, can resemble a more serious infection called orbital cellulitis, in which infection actually penetrates into the eye. Your doctor can distinguish between the two. Periorbital cellulitis is nearly 10 times more common than orbital cellulitis.
Your doctor can also distinguish between periorbital cellulitis and other conditions, such as allergic reactions and conjunctivitis (or pink eye), which also have symptoms of swollen, tender, inflamed eyes.
Periorbital cellulitis causes
Periorbital cellulitis is caused by germs that enter the skin through a cut, scratch, sore, insect bite, dog bite, puncture wound or infected bump such as a stye. The germs can also come from a cold or sinus infection, which means that children who have frequent colds or sinusitis may be more susceptible to periorbital cellulitis. The germs can include common bacteria such as:
Staph infections, from staphylococcus bacteria. This germ is commonly found on the skin or even in the nose. Most of the time, these bacteria live on and in us and cause no problems or result in relatively minor skin infections.
MRSA, a type of staph infection that is more serious because it is resistant to many antibiotics.
Streptococcus bacteria, which often cause a strep throat.
The bacteria that commonly causes pneumonia.
Other infectious organisms such as viruses or fungus.
Is there a vaccine to prevent periorbital cellulitis?
The most common cause of periorbital cellulitis used to be a germ called Haemophilus influenzae type b (Hib). This germ was also once the leading cause of bacterial meningitis in children under five. In 1990, a vaccine was developed to protect against Hib disease and it is now part of routine childhood vaccinations. Therefore, Hib is no longer a common cause of this condition.
How your doctor diagnoses periorbital cellulitis
To diagnose periorbital cellulitis, your doctor will:
Conduct a visual examination, checking your eyes to be sure they move normally and respond to light properly.
Take a medical history and ask questions, such as whether you’ve had any recent infections or injuries, bug bites, scratches or breaks in the skin.
Examine your eye to look at any injury or see if there is a stye or other infected bump that could have led to the condition.
Your doctor may also:
Check your eye pressure to make sure it is normal.
Take a sample of blood to help identify the bacteria involved or to see if there are other infection-related changes in the blood.
Test secretions from the eye in order to identify the bacteria involved.
If your doctor is concerned that you or your child might have orbital cellulitis, which is more serious, they may order a specialized X-ray called a CT (computed tomography) scan. This CT scan will show whether the infection has penetrated beyond the front layer of your eye. Though the two conditions sound similar, they are different and are treated differently.
Periorbital cellulitis treatment
Periorbital cellulitis is usually treated with oral antibiotics for five to seven days. The condition typically responds well and resolves quickly. Your doctor will choose an antibiotic that is effective against the most common germs found in periorbital cellulitis, such as staphylococcus (including MRSA) and streptococcus species. Your doctor may also suggest taking a medication such as acetaminophen or ibuprofen, which help reduce pain, swelling and fever.
If a child with periorbital cellulitis is under a year of age, or the condition is unusually severe, an antibiotic shot or intravenous antibiotics may be required. Children under a year of age may need a brief stay in the hospital while they are being treated.
Can periorbital cellulitis be treated at home?
There are no effective at-home treatments for this condition. You can, however, reduce the risk of this condition. Here are some tips:
Observe good hygiene practices for you or your child.
Clean any scratches, bug bites or injuries near the eye.
Make sure your child is receiving their routine and recommended vaccinations, including Hib.
Treat sinusitis and upper respiratory infections promptly, under a doctor’s care.
Remember, always see your eye doctor if you experience any vision-related or eye problem. If periorbital cellulitis is not treated, it can spread and reach the eye socket, becoming the more serious orbital cellulitis. Your vision is precious, so protect it!
SEE RELATED: Cavernous sinus thrombosis