Endophthalmitis is a severe inflammation of the inside of the eye, usually due to bacterial or fungal infection. Most cases occur after eye surgery, an eye injury or an injection to the eye (such as for medication). Endophthalmitis is considered a medical emergency and should be promptly treated by an experienced eye doctor to avoid permanent vision loss.
In severe cases, endophthalmitis may require enucleation (surgical removal of the eye).
What are the symptoms of endophthalmitis?
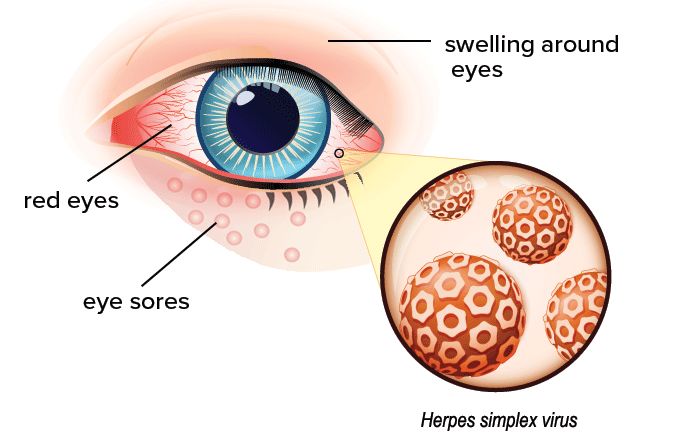
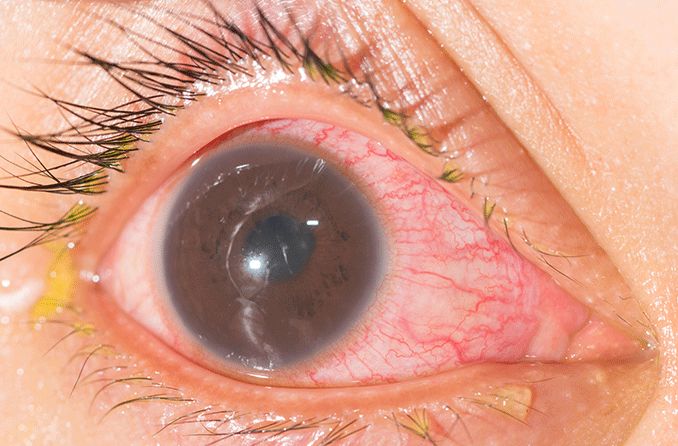
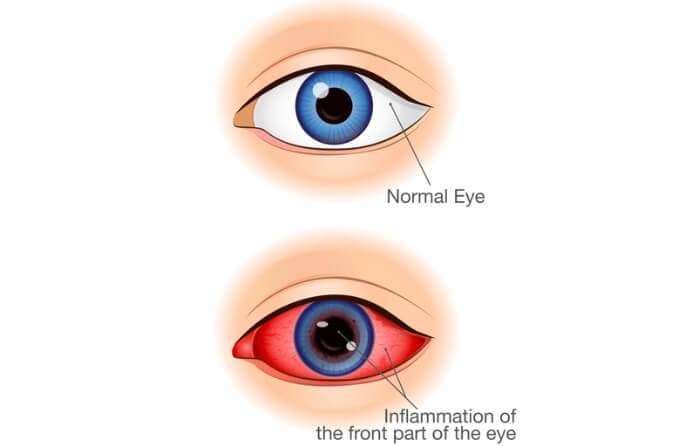
While people with endophthalmitis typically feel well and have no fever, they may experience eye pain and blurred, reduced vision. Signs and symptoms of endophthalmitis include:
- Red, inflamed eyes
- Swollen eyelids
- Sensitivity to bright light
- The appearance of new “floaters” — small, dark floating shapes in the field of vision
- Pus and white blood cells inside the eye
What causes endophthalmitis?
Infection is usually the cause of endophthalmitis. The infection leads to severe inflammation. The infection can arise in several different ways.
Postoperative endophthalmitis
This form is the most common and occurs after surgery (such as cataract or corneal surgery). Postoperative endophthalmitis can occur if bacteria or other pathogens enter the eye through a surgical incision.
Most postoperative endophthalmitis occurs within one week of surgery, but it can appear weeks, months or even years after surgery. Injections into the eye (such as those given for an eye condition called macular degeneration) can sometimes be linked to this condition.
Post-traumatic endophthalmitis
When the eye is injured, punctured or cut due to trauma, germs get in. In this kind of piercing eye trauma, the risk of endophthalmitis is higher if the foreign object remains in the eye. The risk is also higher if there is damage to the lens or if the individual waits more than 24 hours to see a doctor to clean and repair the injury.
Endogenous endophthalmitis
This is endophthalmitis that has an internal cause or origin — in other words, it’s caused by something inside the eye or body, not external factors like trauma, surgery, an eye injection or an external eye infection (such as keratitis that could cause a corneal ulcer that enables external pathogens to enter the eye).
Endogenous endophthalmitis is relatively rare, accounting for an estimated 2% to 8% of all cases of endophthalmitis. It typically is caused by bacteria being spread to the eye from other parts of the body through the blood, and often is associated with a compromised immune system or debilitating diseases.
A liver abscess is the most common source of the infection that causes endogenous endophthalmitis, followed by pneumonia, inflammation of the heart, and infections of the soft tissues of the body (muscles, fat, blood vessels, etc.).
Sterile endophthalmitis
This is a rare type of endophthalmitis that is not caused by an infection. It can be due to an inflammatory or allergic reaction to injections of medications into the eye, and is usually painless. The inflammation slowly resolves and patients usually recover on their own without permanent damage.
What kinds of germs cause infectious endophthalmitis?
Infectious endophthalmitis typically is caused by bacteria of fungi.
Bacterial endophthalmitis
Bacterial endophthalmitis is a type of infectious endophthalmitis resulting after surgery. It can be caused by certain strains of common germs such as staphylococcus and streptococcus, as well as other germs such as klebsiella pneumonia. Researchers have found that most cases occurring after cataract surgery are due to staphylococcus. Penetrating injuries to the eye are often associated with a bacterium called bacillus cereus.
Fungal endophthalmitis
Fungal endophthalmitis is often caused by candida organisms (candida endophthalmitis), which often live on the skin and inside the body without causing any problems. Another common fungus, aspergillus, can also be responsible for this type of infectious endophthalmitis.
A fungus called fusarium has been linked to endophthalmitis in tropical and subtropical parts of the world. However, in 2005-2006, this form of endophthalmitis was associated with a specific brand of lens care solution used by contact lens wearers.
How is endophthalmitis diagnosed?
If you have any symptoms of endophthalmitis, see an ophthalmologist or optometrist immediately. Early detection and treatment of endophthalmitis is essential to prevent vision loss or other potentially devastating outcomes.
Your eye doctor will perform a comprehensive eye exam and closely examine the interior of your eyes to look for clinical signs of the condition. In some cases, an ultrasound test may be performed to better visualize the back of the eye if a significant infection is present.
Your doctor may recommend a procedure called a vitreous tap. After numbing the eye with anesthetic, a tiny needle will remove some of the fluid from the eye. The fluid can be tested to determine which germ is causing the problem.
SEE RELATED: Retina specialist: When should you see one?
How is endophthalmitis treated?
Antimicrobials such as antibiotics or antifungals are necessary to fight the infection in the eye. Types of antibiotic treatments include:
- Intravitreal antibiotics – Antibiotics are injected into the eye with a tiny needle.
- Intravenous antibiotics – Antibiotics can be injected into a vein. This may be necessary for a severe infection, or for an eye infection that started from an infection elsewhere in the body.
- Topical antibiotics – Antibiotics may be applied to the surface of the eye, especially when there has been a traumatic injury.
Surgery may be necessary if the eye has experienced a traumatic injury, and the object or part of the object that caused the injury is still in the eye.
The doctor may need to perform a procedure called a vitrectomy. This procedure removes the infected vitreous membrane that lies in front of the retina and replaces it with oil, saline or another liquid.
Once treatment begins, symptoms will start to improve within a day or two. Eye pain and eyelid swelling will diminish, and if the condition was treated promptly, vision will start to improve as well.
How can you prevent endophthalmitis?
If you are having eye surgery of any kind, make sure to follow all your doctor’s instructions for eye care after your surgery.
Wear protective eyewear such as goggles or eye shields during contact sports or if you work in an industry, such as construction, where you are at a higher risk of traumatic injury.
According to the American Academy of Ophthalmology, individuals with a weak or compromised immune system may be at higher risk of endogenous endophthalmitis. If you are taking medications that weaken your immune system (such as immunosuppressants or steroids), or suffer from diabetes or other conditions that make you more vulnerable to infection, take special care to protect your eyes and make sure you visit your eye doctor for regular checkups.
Remember — Contact an eye doctor immediately if you develop symptoms of this condition.
SEE RELATED: Toxocariasis