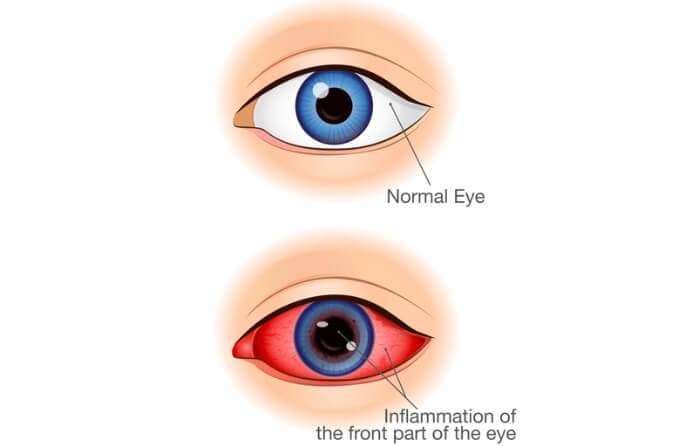
Iritis is inflammation of the iris, the circular structure inside the eye that surrounds the pupil and gives your eyes their color. The inflammation usually develops quickly and typically in just one eye, although both eyes can be affected.
There are potentially serious complications associated with iritis, including cataracts, glaucoma, retinal damage and vision loss. Prompt diagnosis and treatment by an eye doctor is advised.
What is the iris?
The iris is part of the pigmented middle layer of the eye known as the uvea, which includes the iris, ciliary body and choroid. The iris is the most anterior portion of the uvea; for this reason, iritis also is known as anterior uveitis.
A thin, circular structure composed of connective tissue and muscle, the iris expands and contracts in response to light, helping us to see clearly.
In bright light, the iris dials back the pupil, making it smaller.
In dim light, the iris opens up the pupil wide to let in as much light as possible.
In addition to its visual function, the iris also determines eye color, based on the amount of melanin it contains.
Melanin is a dark brown pigment that’s also found in skin and hair. The higher the level of melanin in the iris, the darker your eye color will be.
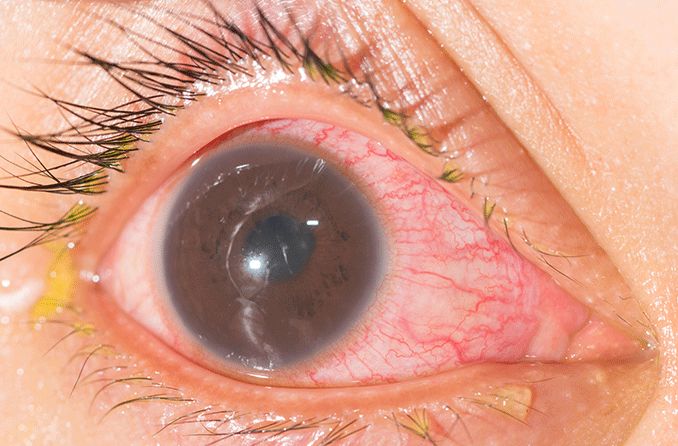
Iritis symptoms
Signs and symptoms of iritis include:
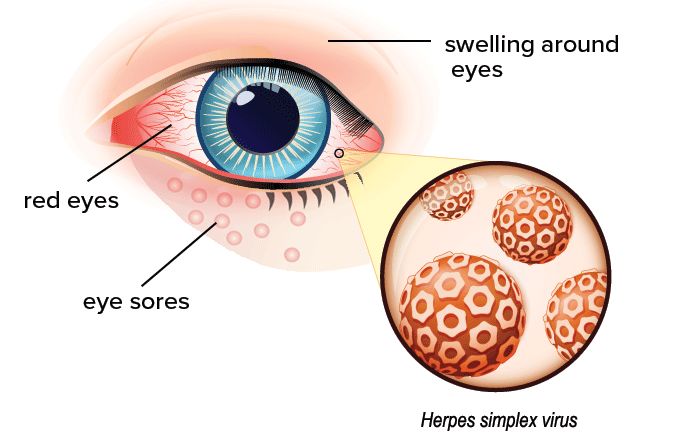
- Red eyes
- A small or oddly shaped pupil
- Eye pain
- Headache
- Blurry vision
- Photophobia (sensitivity to light)
- Pain in the brow area
If the onset of iritis is sudden (hours or days), it’s called acute iritis. Chronic iritis develops more gradually and/or lasts more than six weeks.
Iritis can lead to severe vision problems, including blindness, so you should see an eye doctor as soon as possible if you start to experience symptoms of iritis.
SEE RELATED: Eye inflammation
Causes of iritis
Often no specific cause of iritis is found, but there are several reasons it can develop.
Causes of iritis are broken down into two general categories: traumatic and non-traumatic.
Traumatic iritis
Traumatic iritis occurs as the result of injury to the eye, such as blunt force trauma that causes swelling, a penetrating injury, burns and exposure to toxic chemicals.
With treatment, traumatic iritis may take a couple of weeks for the eye to heal and the iritis to clear up completely. However, there still is a possibility of permanent vision damage, depending on the severity of the injury.
Non-traumatic iritis
Non-traumatic iritis is associated with certain infectious diseases or medical conditions. These include:
- Inflammatory bowel disease
- Psoriasis
- Lyme disease
- Herpes simplex
- An outbreak of herpes zoster (eye shingles) on the face
- A weakened immune system or autoimmune disorder
- Tuberculosis
- Sarcoidosis
- Systemic lupus erythematosus
- Toxoplasmosis
- Syphilis
- HIV/AIDS
- Certain types of arthritis (include juvenile rheumatoid arthritis)
- Reiter's syndrome (the combination of arthritis, uveitis, and conjunctivitis)
Chronic iritis also has been linked to smoking. Researchers have concluded that compounds in cigarette smoke stimulate inflammation of blood vessels and may be a contributing factor to disruption of the immune system leading to iritis.
Iritis caused by an infectious disease will heal once the infection is cured. Iritis that’s connected to a systemic disease may be chronic, recurring as the disease worsens and fading as it improves.
Non-traumatic iritis may linger for weeks or months before it resolves.
Iritis diagnosis and treatment
Iritis is diagnosed by an eye care professional using a three-pronged approach.
The first step is an external examination of the eye using a light to observe the pupil(s), any redness that’s present and any signs of discharge.
Next comes a visual acuity test using an eye chart and other standard measures to see how sharp the vision is.
Finally, a slit lamp examination is done to confirm the diagnosis. A slit lamp is a special microscope designed for eye exams that allows the doctor to see white blood cells and flare, or particles of protein, in the vitreous humor (fluid within the eyeball).
The eyes are dilated for this part of the exam, so you may want to have someone who can help you get home accompany you to the appointment.
Once diagnosed, the goals of treatment for iritis are:
- Reduction of inflammation and pain
- Prevention of damage to the eye
- Restoration or preservation of vision
In general, the course of treatment is determined by the severity of the iritis and how well the eye responds to the initial treatment prescribed.
Iritis is treated with prescription medications, especially eye drops. Drops that dilate the pupil and relax the iris muscles also can help ease discomfort.
Steroid eye drops may be prescribed on a short-term basis to reduce inflammation. If the eye hasn't improved within a week, steroid pills or injections around the eye may be an option.
Mild, over-the-counter pain relievers like acetaminophen and ibuprofen may help relieve discomfort associated with iritis.
If the affected eye is sensitive to light, sunglasses or glasses with photochromic lenses may be recommended.
If you suspect iritis, see your eye doctor
If you are experiencing symptoms of iritis, see an eye doctor near you soon. Don't wait.
If you are diagnosed with iritis, carefully follow your eye doctor’s instructions. Proper care is essential to prevent permanent vision damage, so be sure not to miss any scheduled follow-up appointments.
READ NEXT: Iridocyclitis