Horner’s syndrome is a rare disorder that affects the eye and nearby tissue on one side of the face. This condition can appear at any point in someone’s life; fewer than 1% of people are born with it. Typically, problems that arise from Horner’s syndrome don’t harm a person’s vision or health.
This disorder affects males and females equally and can happen in any age group, ethnic group or geographic location.
Horner’s syndrome is also known as Horner syndrome, Bernard-Horner syndrome, oculosympathetic palsy or von Passow syndrome. Horner’s syndrome is named after Swiss ophthalmologist Johann Friedrich Horner, who discovered and documented the disorder in 1869.
Horner’s syndrome symptoms
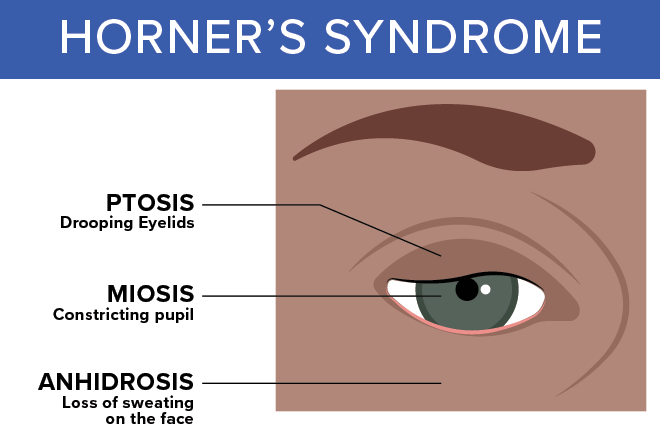
Several symptoms accompany Horner’s syndrome:
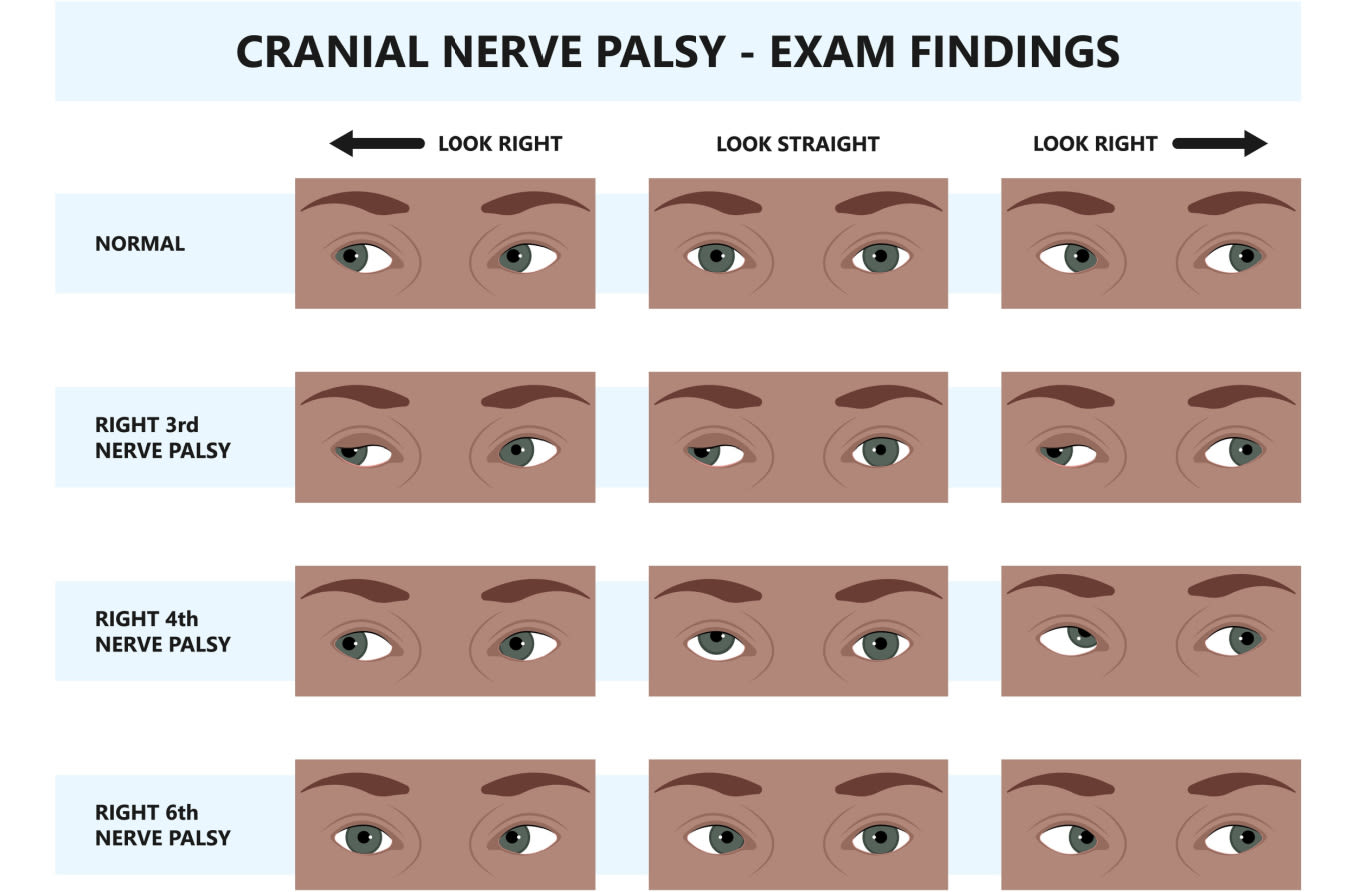
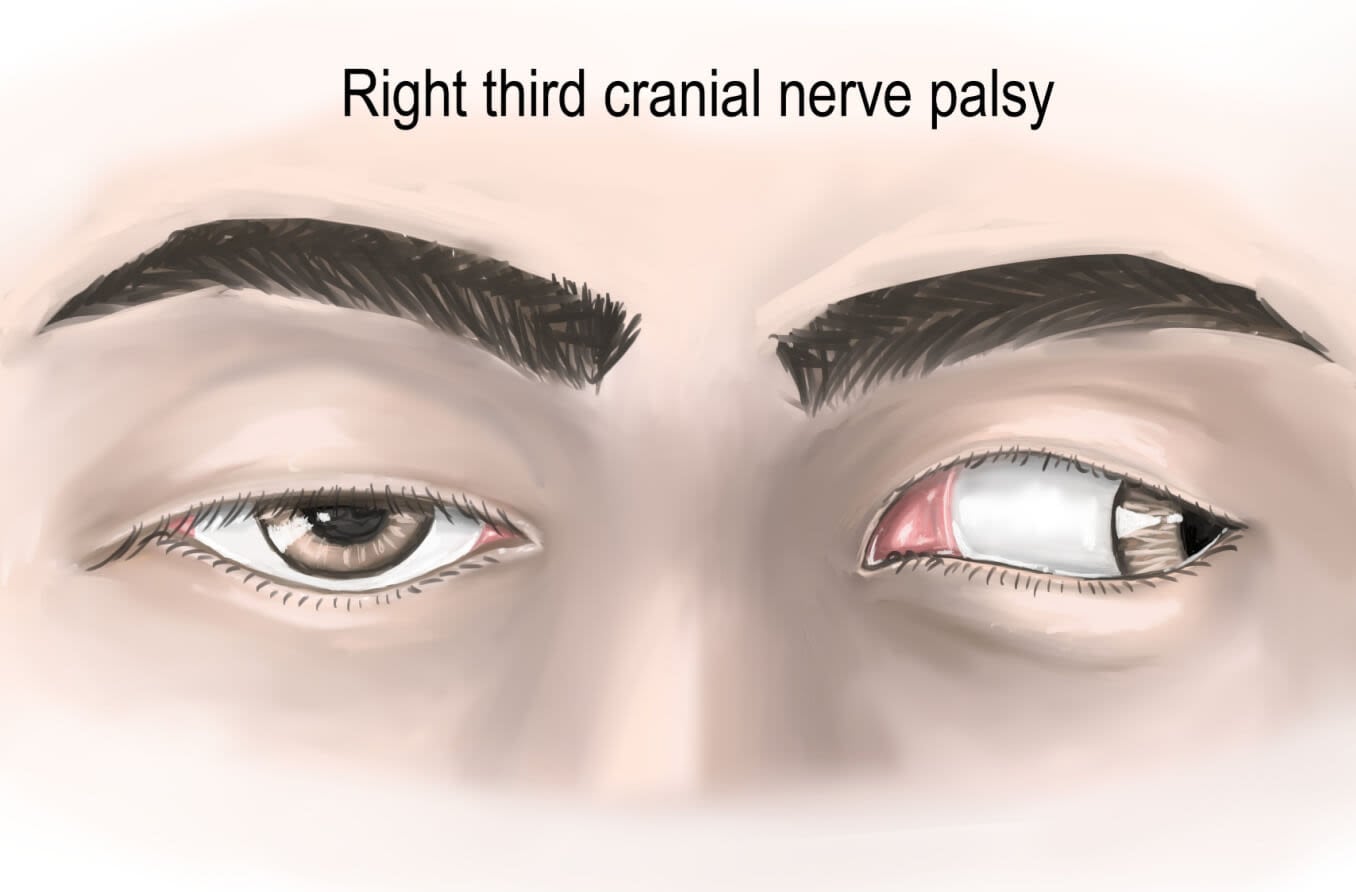
Drooping of the upper eyelid on the affected side
Constricted pupil in the affected eye (miosis), leading to unequal pupil size (anisocoria)
Absence of sweating (anhidrosis) on the affected side of the face.
Inability to open or completely close the eyelid
Facial flushing
Headaches
Pain
Someone with Horner’s syndrome also may experience sinking of the eye into its cavity (enophthalmos) and a bloodshot eye.
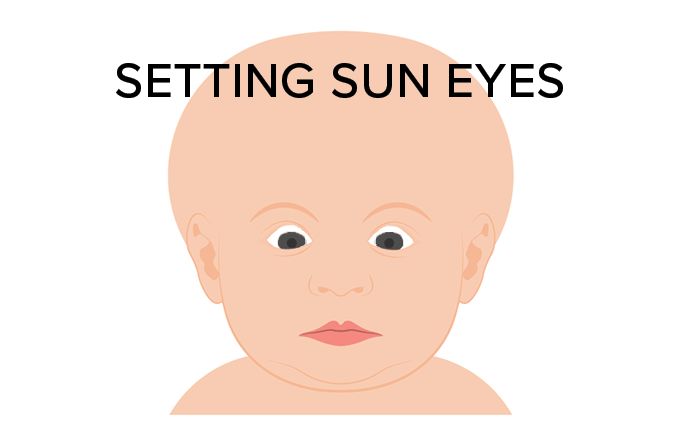
If Horner’s syndrome appears before age 2, the iris (colored part) of the affected eye may be lighter in color than the unaffected eye (iris heterochromia). People who are diagnosed with Horner’s syndrome after age 2 typically don’t have differences in eye color.
While vision and health normally aren’t harmed by Horner’s syndrome, the nerve damage that triggers this disorder may be a sign of other health problems.
Symptoms that may accompany Horner’s disease, but are not directly caused by it, include:
Vertigo, coupled with nausea and vomiting
Lack of muscle control and coordination
Arm pain, weakness and numbness
Neck and ear pain on one side of the body
Hoarseness
Hearing loss
Bowel and bladder problems
Overreaction to stimulation
Horner’s syndrome causes
Horner’s syndrome results from damage to the sympathetic nerves, which regulate dilation of our pupils and raising of our eyelids. Causes may include:
Snake or insect bite
Stroke
Birth trauma to the neck and shoulder
Trauma or surgery involving the neck, upper spinal cord or chest
Blood clot
Migraines or cluster headaches
Cyst in the spinal cord
Lymph node inflammation or growths
Tear in the carotid artery, which supplies blood to the head and neck
Demyelinating diseases, which are disorders of the nervous system
Chiari malformation, which affects the part of the brain that controls balance
Tumor In the brainstem, hypothalamus section of the brain, upper spinal cord, neck, eye, abdomen, chest cavity or upper part of the lung
Some cases of Horner syndrome occur for no apparent reason, according to the National Organization for Rare Disorders. In other cases, the disorder may be genetically inherited.
In children, one of the most common causes of Horner’s syndrome is neuroblastoma. Neuroblastoma is a cancer that starts in nerve cells (called neuroblasts) of the sympathetic nervous system.
Congenital Horner’s syndrome
Horner's syndrome is generally acquired in adulthood. Fewer than 5% of cases of this disorder are classified as congenital Horner’s syndrome. A disease or condition that is present at birth is said to be congenital.
Congenital Horner’s usually is associated with trauma suffered during birth or shortly before birth, as well as with tumors in children and cardiothoracic surgery performed on a newborn. Cardiothoracic surgery involves procedures on the heart, lungs and esophagus. In a few rare instances, congenital Horner’s syndrome appears to be an inherited genetic trait.
Most cases of congenital Horner’s syndrome result from damage to nerves known as the cervical sympathetics. The cervical sympathetic nerves control several functions in the eye and face such as pupil dilation and facial sweating. These nerves can be damaged as a result of birth difficulties, surgery or accidental injury, as well as benign or cancerous tumors. For some people with congenital Horner’s syndrome, their carotid artery has not developed properly (agenesis).
Horner’s syndrome diagnosis
An eye doctor may be able to confirm Horner’s syndrome with a special eye test. Furthermore, tests may be needed to pinpoint the cause. These tests may include:
MRI of the head
Ultrasound of the carotid artery
CT scan of the chest
Chest X-ray
Blood tests
Angiogram, which provides a view of the arteries
Eye drop tests
The eye drop tests may involve two steps:
Applying eye drops that contain small amounts of cocaine or apraclonidine to both eyes.
Performing another test 48 hours later if Horner’s syndrome is suspected. In this test, hydroxyamphetamine drops will be applied to both eyes.
The eye doctor will see how the pupils react to the drops. That reaction will determine whether Horner’s syndrome is present. Then, other tests may be required, such as an MRI or CT scan, to figure out what’s causing the disorder.
If a child is diagnosed with Horner’s syndrome, the doctor may order more tests, such as X-rays or urine tests, to find out whether the patient has neuroblastoma or any abnormalities in the abdomen, brain, chest or neck.
Someone who suddenly experiences the following symptoms associated with Horner’s syndrome should seek emergency care:
Impaired vision
Dizziness
Muscle weakness or lack of muscle control
Severe, sudden headache or neck pain
Horner’s syndrome treatment
There is no treatment for Horner’s syndrome. The lingering effect is often a slightly droopy eyelid. That droopiness may be corrected by cosmetic surgery or eye drops.
Also, there are no complications from Horner’s syndrome. But complications may be triggered by the cause of the disorder.
While there is no treatment for Horner’s syndrome itself, the underlying cause can be treated.
While Horner’s syndrome itself “will not damage the eye or cause loss of vision, it could be a signal of damage to one of the structures along the nerve. It is important to find out where the damage is and what is causing it because sometimes it can be serious,” according to Manchester University’s Royal Eye Hospital.
Addressing the underlying cause may help alleviate symptoms of Horner’s syndrome, including discomfort and reduced nerve function.
Importance of eye exams
Regardless of whether you’re coping with Horner’s syndrome or another eye condition, or even if there are no obvious problems with your eyes, it’s important to visit your optometrist or ophthalmologist to undergo regular eye exams.
READ NEXT: Rare eye diseases: What causes them, and how are they treated?