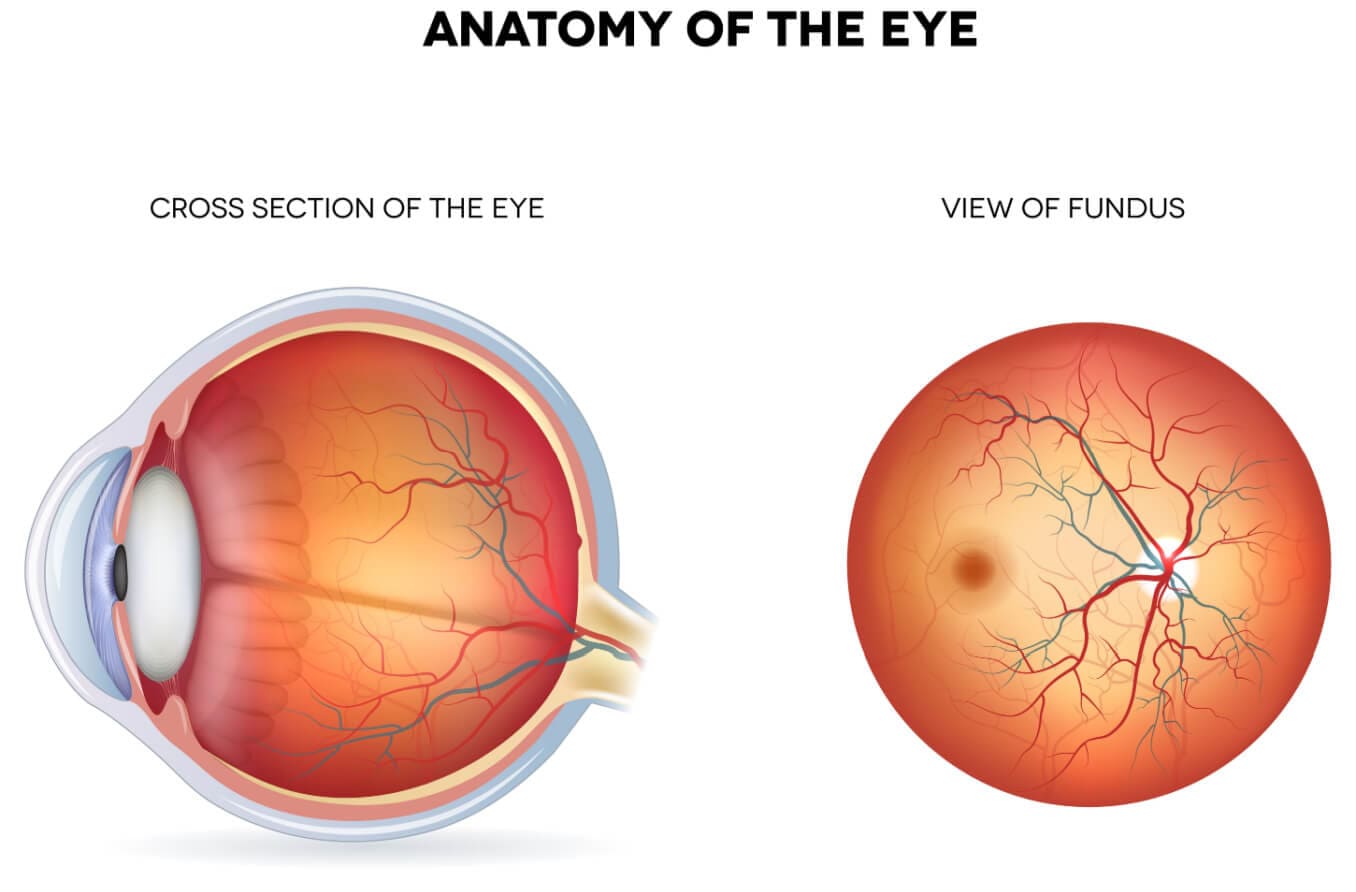
What is the fundus?
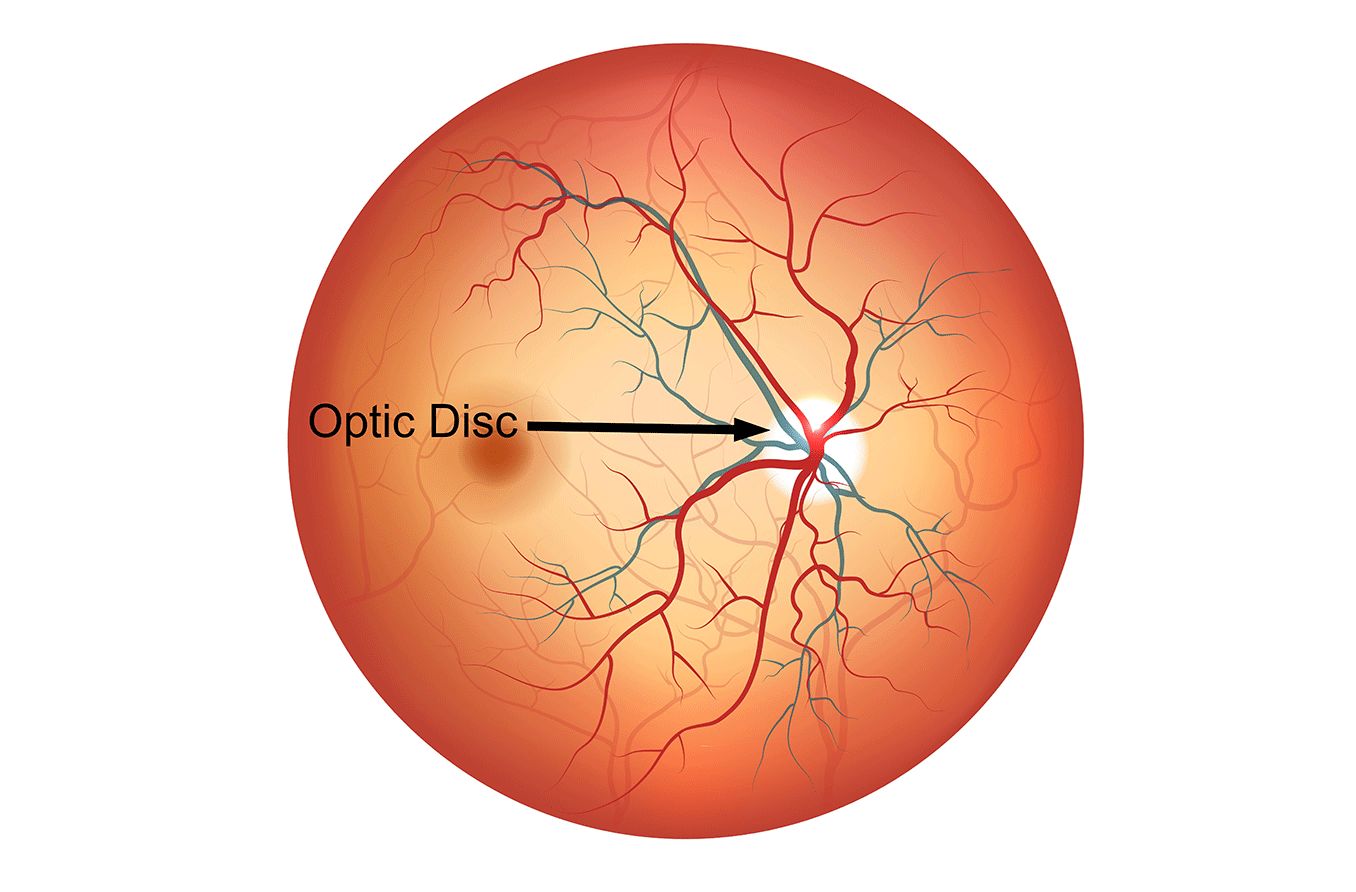
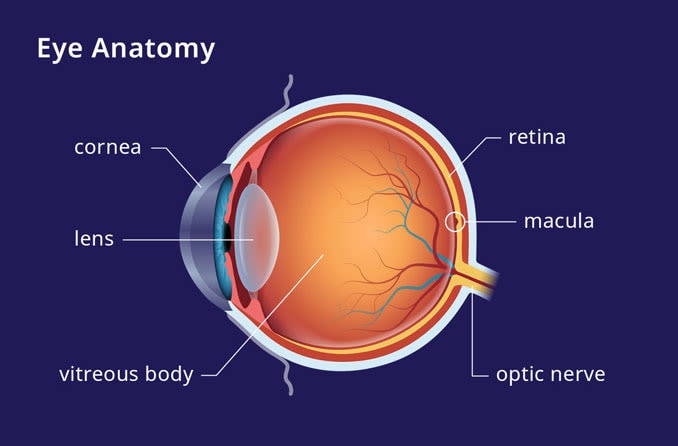
The back part of the inside of the eye is called the fundus. It is where the retina, macula, fovea, choroid and optic disc, as well as blood vessels, are located. A fundus exam can be performed to detect a variety of eye conditions.
The term fundus is used to describe the structure that is farthest back from the opening of any hollow organ. Other organs that have a fundus include the bladder, gallbladder, stomach and uterus.
Fundus anatomy
There are many parts of the eye that are located in the fundus. They include:
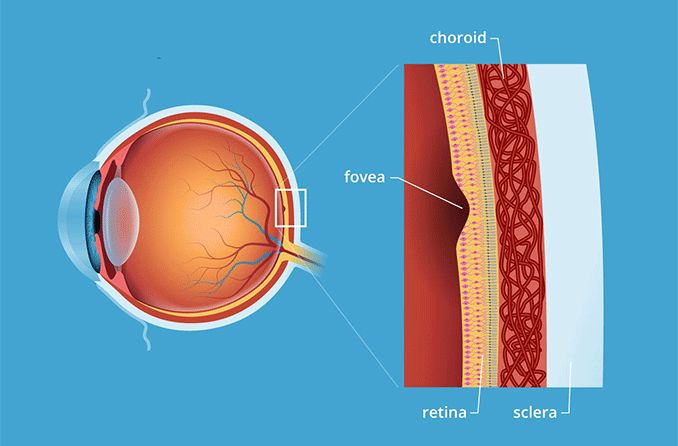
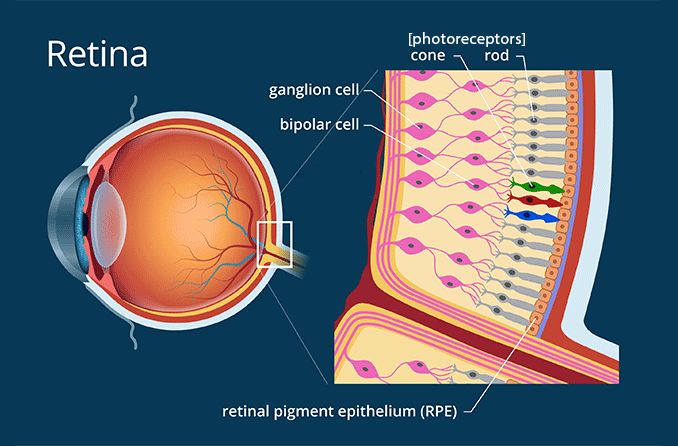
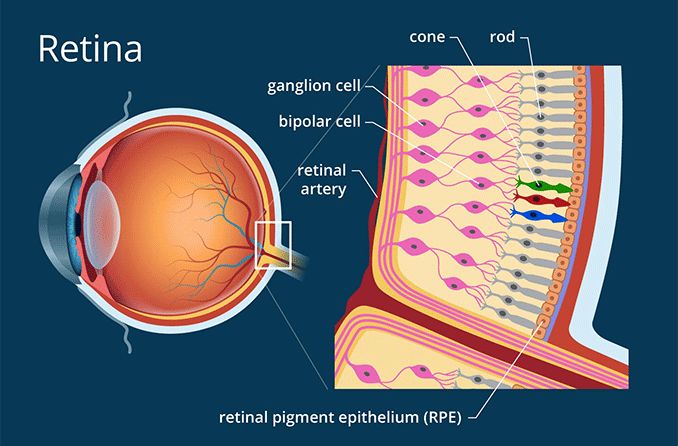
Retina – The layer of cells on the back of the eye. These cells are called photoreceptors. Photoreceptors convert light into electrical signals, which are sent to the brain. This allows you to see images.
Macula – This is the center area of the retina. It is responsible for your central vision, or what you can see that is right in front of you. It also allows you to see details of the things you look at.
Fovea – The small depression inside the macula. This is where your vision is the sharpest.
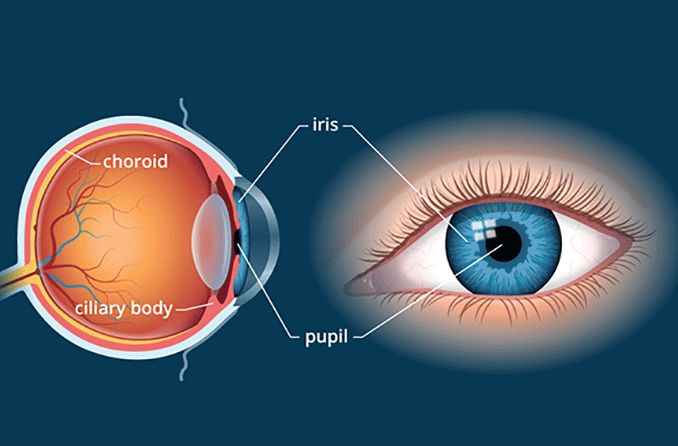
Choroid – The part of the eye located between the retina and the sclera (the white part of the eye). It contains blood vessels that send nutrients to the eye.
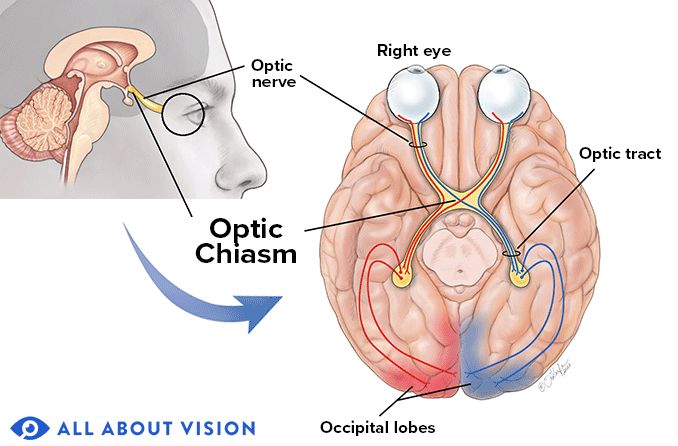
Optic disc – The area where the retina connects to the optic nerve. The optic nerve connects to the brain and is critical to your ability to see.
Retinal blood vessels – The blood vessels that support the inner retina. The central retinal artery and its branches carry blood to the retina, supplying it with oxygen and nutrients. The central retinal vein and its branches carry blood away from the retina, removing carbon dioxide and waste.
Function of the fundus
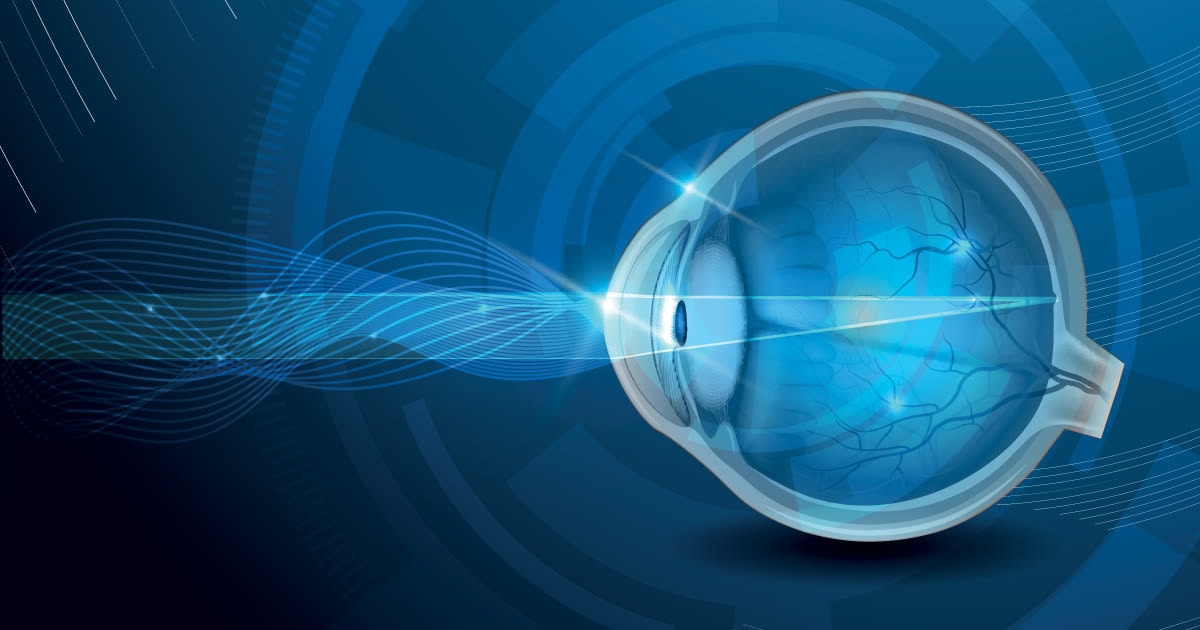
The cornea and the lens in the front of the eye help focus the light that enters the eye. When the light hits the fundus, the retina then converts that light into electrochemical impulses. These impulses then go to the brain via the optic nerve. Healthy function of the parts of the back of the eye are important in being able to see.
Fundus exam
In order to examine the fundus, an eye doctor can perform a fundoscopy. This is also known as an ophthalmoscopy. There are three different types.
Direct ophthalmoscopy
This exam is done with the patient seated in a dark room. A doctor uses an ophthalmoscope to shine a light through the pupil. The ophthalmoscope has different lenses that allow the doctor to see the back of the eye.
Indirect ophthalmoscopy
This exam is especially useful when a doctor is looking for a detached retina, retinal tear or a retinal hole.
The patient lies down or is reclined. Eyedrops are used to dilate the pupil. Dilating the pupil allows the doctor to get a better view of the retina. Your eye doctor will use a tool called a binocular indirect ophthalmoscope (BIO).
This looks like a headband with a built-in light and lens. The doctor will hold an additional lens to view the back of the eye. The patient will be asked to look in different directions while the doctor holds the lens.
During the exam, the doctor might apply pressure to the eye using a probe. The pressure might feel slightly uncomfortable but not painful.
Slit-lamp ophthalmoscopy
In this exam, the doctor can see the back of the eye in a similar way as an indirect ophthalmoscopy. But there is a higher magnification in a slit-lamp ophthalmoscopy.
It is performed with the patient seated. Eye drops may be used to dilate the pupil. An instrument called a slit lamp is placed in front of the patient. The doctor has the patient rest their chin and forehead on the instrument to keep the head from moving.
A microscope on the slit-lamp is used along with a lens that the doctor places close to the eye in order to view the back of the eye.
The bright light that is used during an ophthalmoscopy may be a bit uncomfortable. However, the exam is not painful. The eye drops used to dilate the eyes may sting a little bit. The exam takes about five to 10 minutes.
Because your blood vessels can be seen during a fundus exam, a variety of vascular conditions can be detected. Some of these conditions include diabetes, hypertension and even endocarditis (inflammation in the heart).
Fundus photography
In addition to a fundoscopy, a fundus camera can be a useful aid during a comprehensive eye exam. This camera is able to take photographs of the fundus.
Before the photo is taken, the patient will be given eye drops to dilate the eyes. The patient then places their chin and forehead in the appropriate places on the camera to keep their head in place.
The patient will be asked to focus on a green light while the doctor adjusts the camera and takes the photo. This is a non-invasive procedure and can assist in detecting a variety of health issues.
Conditions that can affect the fundus
There are many conditions that can affect the fundus. They include, but are not limited to:
Diabetic retinopathy
This is a type of retinopathy that can occur in those who have had uncontrolled diabetes for a long period of time. Signs of diabetic retinopathy during a fundus exam include microaneurysms, hemorrhages and capillary changes.
Symptoms include floaters, blurry vision and partial vision loss. Diabetic retinopathy is the leading cause of vision loss in adults in the Western population.
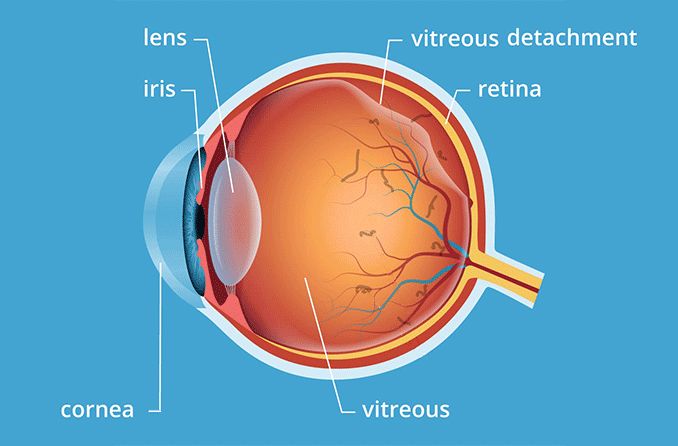
Detached retina
This is a condition in which the retina detaches from the back of the eye. A detached retina happens when the vitreous pulls on the retina and tears it. Then the fluid goes under the tear, detaching the retina.
This can sometimes happen in older individuals when the vitreous begins to thin and shrink.
Symptoms include floaters, a shadow in your peripheral vision, seeing flashes of light or seeing a gray curtain covering part of your vision. Vision loss is possible.
Retinal vein occlusion
Retinal vein occlusion is a condition that occurs when there is a partial or total blockage in a vein that moves blood away from your retina. Those with conditions that cause hardened arteries from cholesterol or fat buildup (diabetes, glaucoma and high blood pressure) are at a higher risk.
Symptoms include floaters, pain in the eye, blurry vision and vision loss.
Age-related macular degeneration (AMD)
Age-related macular degeneration is a disease that causes central vision loss. Your peripheral vision is not affected. There are two types: dry and wet AMD. Dry AMD is most common and causes gradual vision loss. Wet AMD is less common but can cause faster vision loss.
Those with AMD usually do not know they have it until their vision becomes blurry. It is one of the main causes of vision loss in those over 50 years old.
Macular hole
A macular hole is exactly what it sounds like: a hole in the macula. Those who are most at risk include older individuals, those who are very nearsighted and those who have had trauma to the eye.
Symptoms include blurry vision, not being able to read small print and distorted vision. Vision loss, especially central vision loss, is possible.
Macular pucker
Wrinkles or bulges that form on the macula are called macular pucker — or epiretinal membrane (ERM). ERM usually occurs in older individuals when the vitreous sticks to the retina. This causes scar tissue, and the macula becomes wrinkled.
Symptoms include having problems with your central vision, such as being unable to see details, as well as distorted vision.
Stargardt Disease
Stargardt disease is an inherited disease that is also known as juvenile macular dystrophy or fundus flavimaculatus. It is a type of macular degeneration that occurs in childhood.
Vision loss usually starts to occur in the first decade of life. The central vision is affected, but the peripheral vision typically remains unaffected.
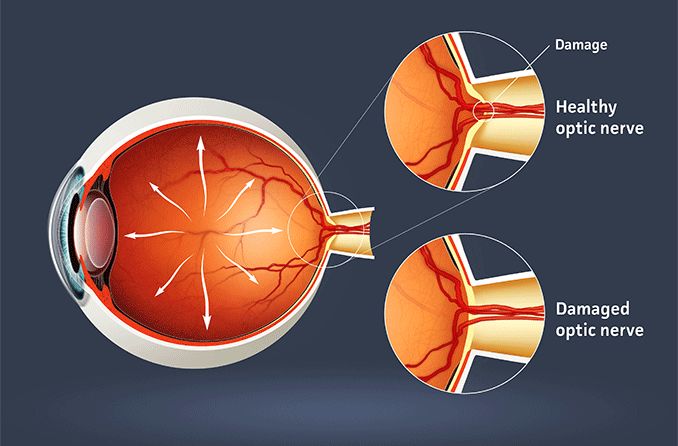
Glaucoma
Glaucoma is a group of conditions that damage the eye’s optic nerve leading to progressive vision loss. Glaucoma is usually due to fluid buildup in the eye. The high pressure from the fluid buildup damages the optic nerve. It can also occur with normal pressure, however.
Some people do not have any symptoms early on. Others may have eye pain, headaches, impaired vision, seeing halos, nausea or red eyes. Early detection is important to help prevent blindness.