Do I have to get the air puff test during my eye exam? No, the air puff test is not the only option these days for measuring your eye pressure. In fact, your eye doctor might have stopped using the air puff test altogether.
It's easy to understand why you and countless others would rather skip the air puff test. For decades, that quick "poof" sound of air being shot into your eye has probably been the most annoying, dreaded part of your eye exam.
But what is the air puff test, how does it work and are there alternatives? We've got the answers to frequently asked questions about the air puff test.
What is the air puff test?
Traditionally, ophthalmologists and optometrists have gauged the pressure inside your eyes using the air puff test, formally known as “non-contact tonometry” or “air puff tonometry.”
The test helps determine whether you have glaucoma or are at high risk for developing glaucoma, a condition that harms the optic nerve and can cause blindness.
According to the American Academy of Ophthalmology (AAO), glaucoma normally happens when fluid builds up in the front part of your eyes, causing your eye pressure (known as intraocular pressure, or IOP) to go up.
How does the air puff test work?
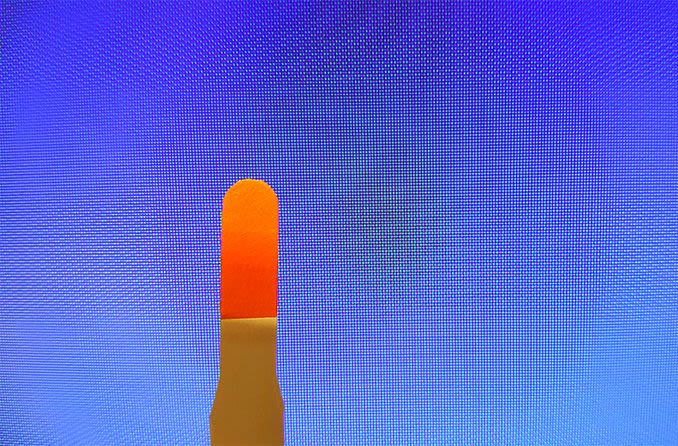
The air puff test starts with a patient seated at the tonometry machine with their chin atop the equipment’s chin rest. As the patient stares at a light inside the machine, a small burst of air is “puffed” into each open eye.
Although this might be a little uncomfortable and unnerving, it’s not painful; nothing but the puff of air touches the eye. Numbing eye drops aren’t required for the air puff test.
The puff of air slightly flattens the cornea, according to the U.S. National Library of Medicine. How much the cornea flattens depends on your eye pressure.
Based on your eyes’ response to the puffs of air, the tonometer calculates the pressure inside each eye. A high level of pressure might mean you’re at risk of developing glaucoma or already have the condition.
According to the AAO, “Each person’s eye pressure is different, and there is no single correct pressure for everyone.”
Since glaucoma usually isn’t accompanied by symptoms, it’s quite possible to have the condition without realizing it.
According to the Glaucoma Research Foundation, it’s estimated that more than 3 million Americans have glaucoma, and about half of them are unaware of it.
That’s why it’s critical for an eye doctor to perform a glaucoma test as part of a comprehensive eye exam, and that you get eye exams regularly, even if you aren’t sure you need one.
WHEN WAS YOUR LAST EYE EXAM? Find an eye doctor near you and schedule an appointment.
How effective is the air puff test?
The air puff test is not the best way to measure eye pressure, according to the University of Michigan Health System, but it is a simple way to check eye pressure, and it’s the easiest way to test eye pressure in children.
Are there alternatives to the air puff test?
Many eye doctors have ditched the air puff test and switched to other, more reliable methods of tonometry to measure eye pressure and help detect glaucoma.
One of these methods is applanation (Goldmann) tonometry. The National Library of Medicine outlines the key steps in what’s considered the standard, most accurate test for measuring eye pressure:
- An eye doctor or assistant numbs the surface of each eye with eye drops.
- You rest your chin and forehead against the tonometer to keep your head still during the procedure.
- The eye doctor or assistant asks you to keep your eyes open and look directly ahead.
- The eye care professional touches your cornea with the tip of the tonometer.
- The eye doctor or assistant looks through an eyepiece and adjusts a dial on the machine to read your eye pressure.
The second alternative to the air puff test is called electronic indentation tonometry.
According to the National Library of Medicine, an eye care professional measures your eye pressure during this test, with a handheld, pencil-shaped device after numbing eye drops have been administered to ease discomfort. The professional touches the surface of your cornea with the device and records your eye pressure.
Although the University of Michigan Health System describes this test as “very accurate,” the results might differ from those supplied by the more precise method: applanation tonometry.
Is just one of these tests enough to diagnose glaucoma?
No. According to the AAO, checking your eye pressure isn’t enough to determine whether you have glaucoma. An eye doctor also needs to:
- Look at the drainage angle of your eye to see whether it’s blocked. That blockage can cause a buildup of fluid, leading to a potential increase in eye pressure.
- Examine your optic nerve for damage.
- Take a picture or computer measurement of your optic nerve.
- Test your peripheral (side) vision.
- Measure the thickness of your cornea.
DOES GLAUCOMA RUN IN YOUR FAMILY? Find an eye doctor near you and book a comprehensive eye exam.