What is pneumatic retinopexy?
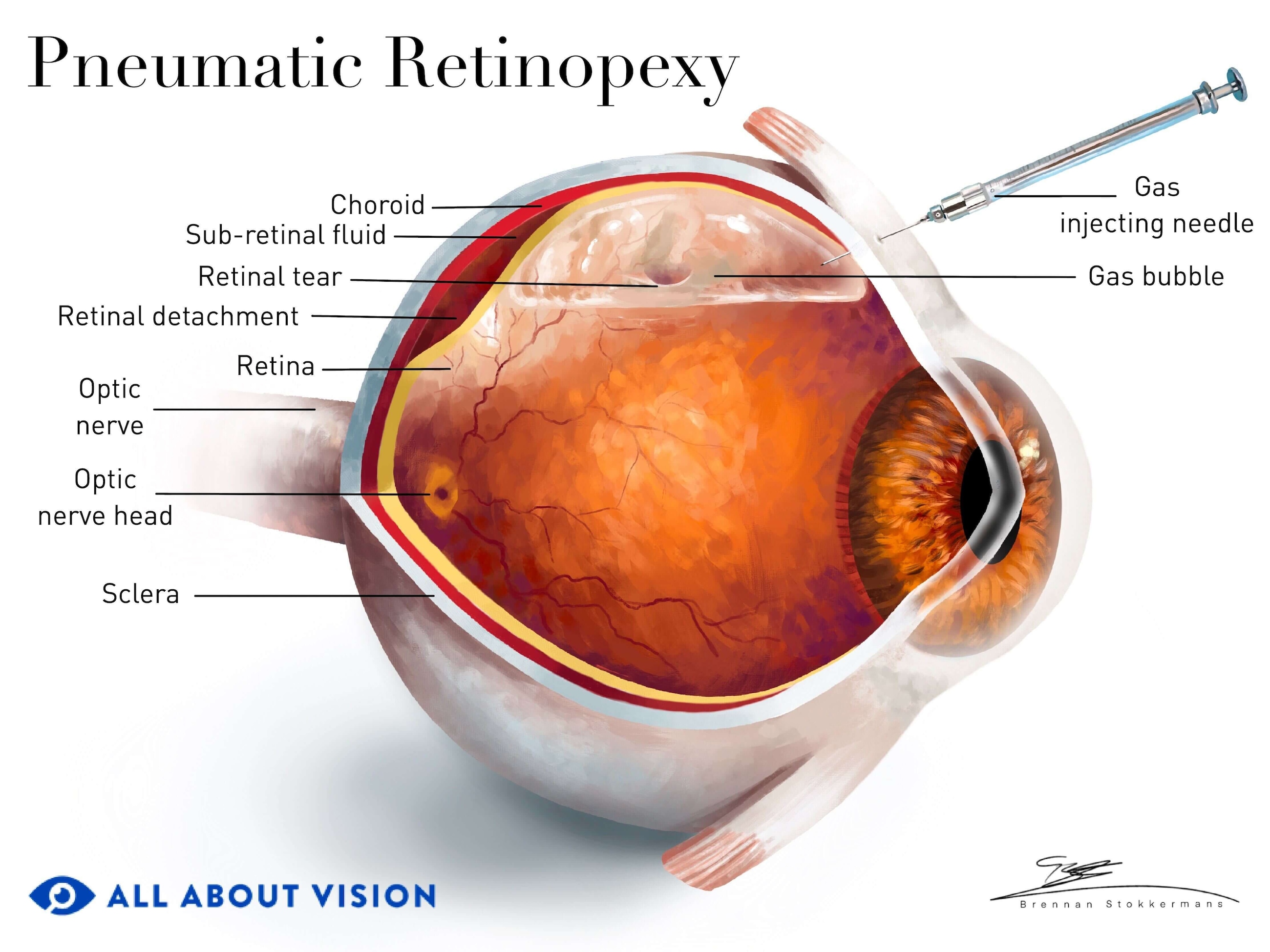
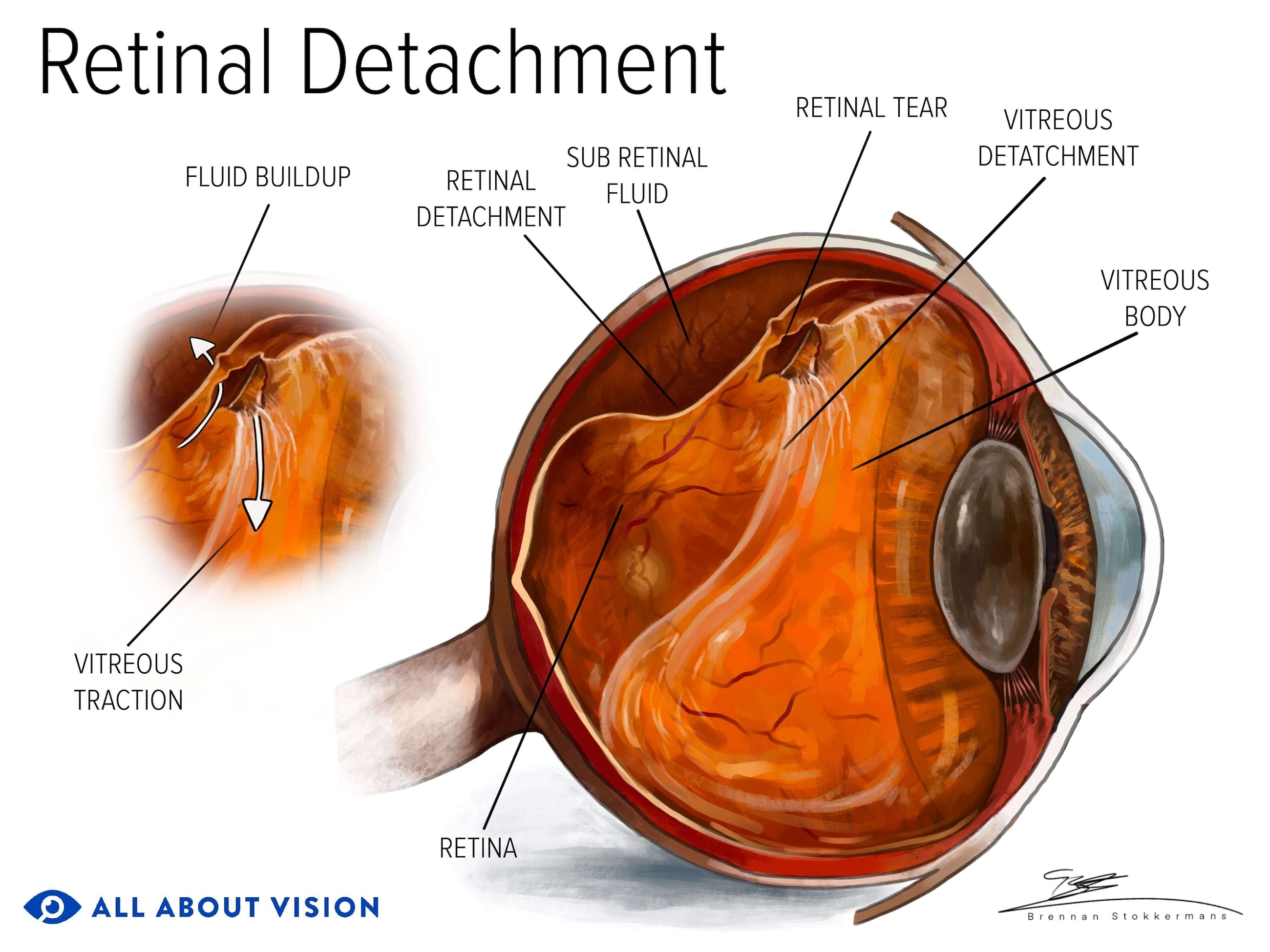
Pneumatic retinopexy is an in-office treatment to repair a rhegmatogenous retinal detachment (RRD). RRD can occur if fluid seeps under the retina, causing it to pull away from the back of the eye. A gas or air bubble is injected into the eye to help hold the retina in place and aid in fluid reabsorption.
The injected bubble will usually stay in the eye for about two to six weeks. Your vision will be blurry during this time. It is important to note that airplane travel is not allowed while the air or gas bubble is in the eye. Higher altitude will cause the bubble to expand, which can cause complications.
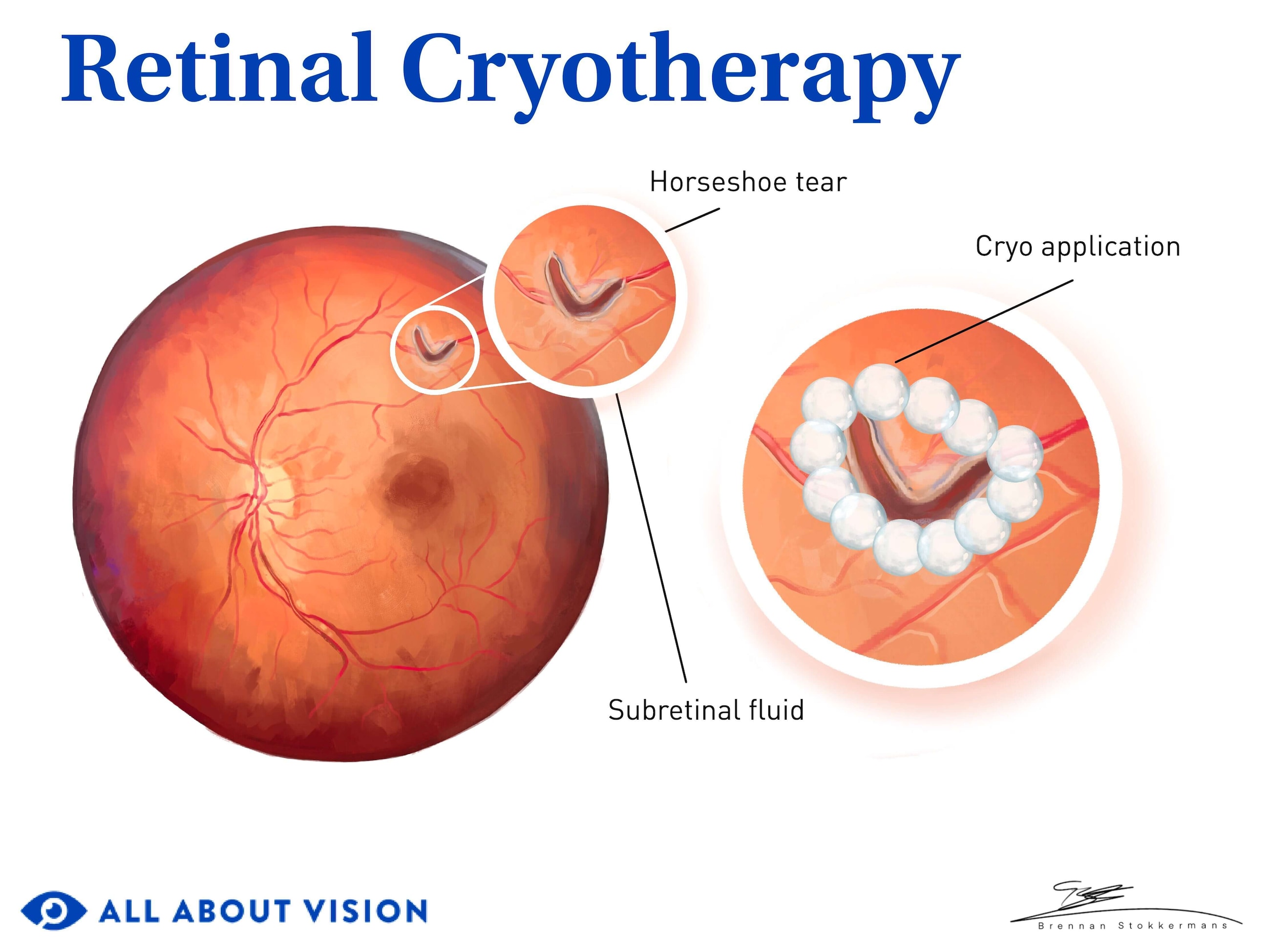
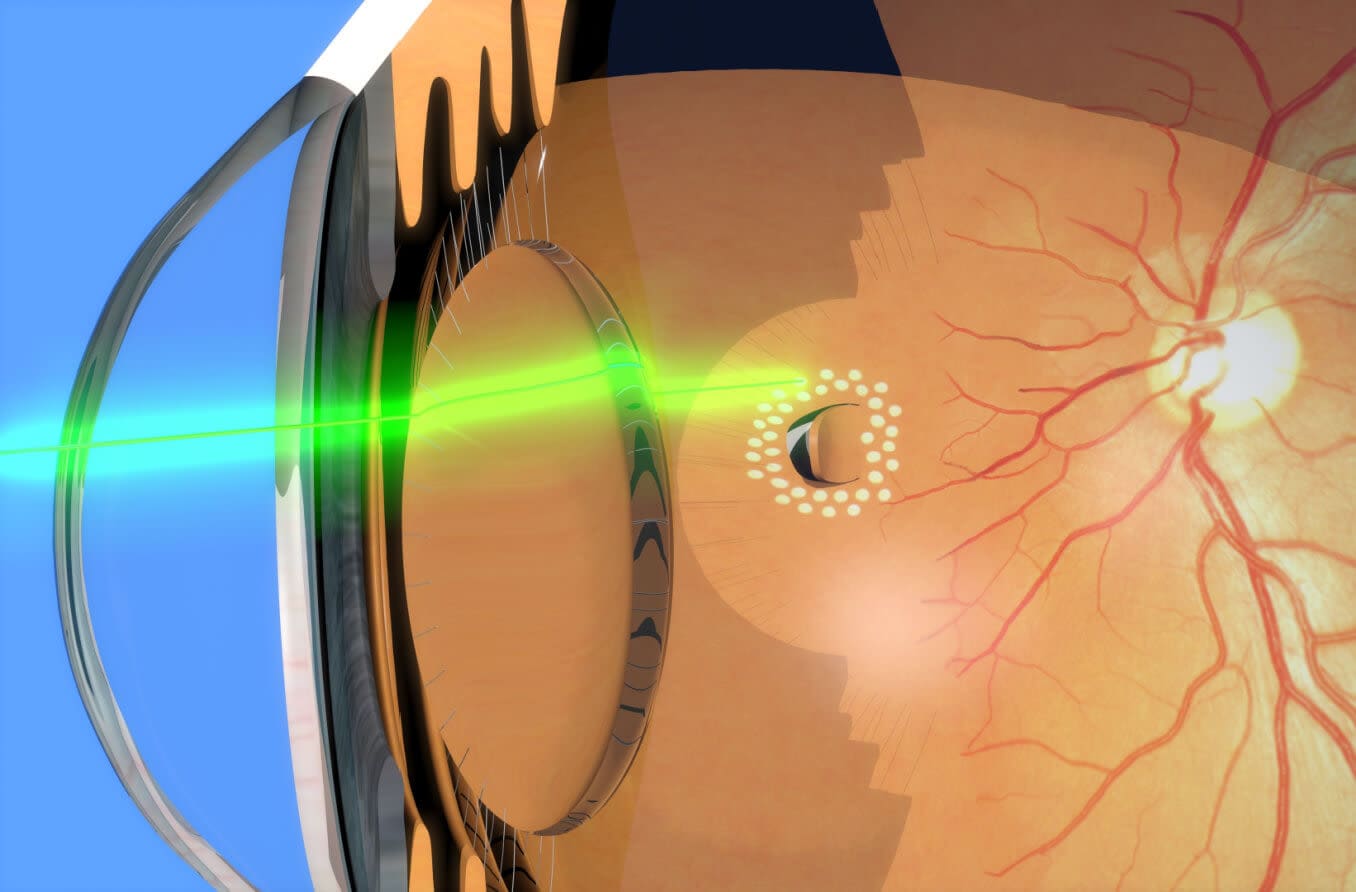
Pneumatic retinopexy is typically done at the same time as laser retinopexy, cryopexy (a freezing probe procedure) or both. These treatments help to reattach the retina by creating scar tissue adhesions around the area of the retinal break.
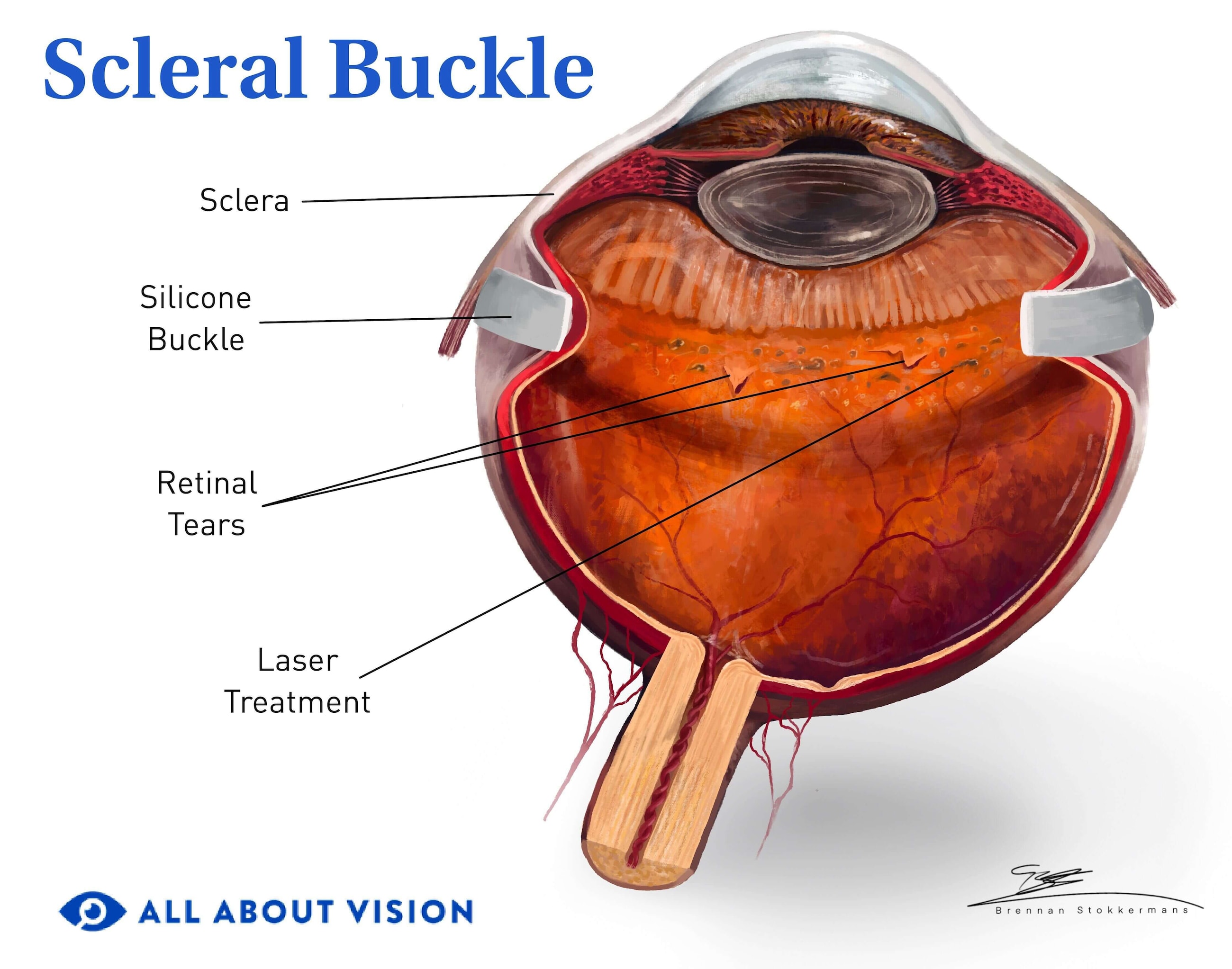
This procedure may not be a treatment option for some individuals. For example, those with certain eye or medical conditions or a break in the lower half of the retina may not be good candidates. However, it is an outpatient procedure and does not require an incision. So it may have several potential benefits over surgeries that require an operating room, such as pars plana vitrectomy or scleral buckle.
Advantages of pneumatic retinopexy include:
Faster overall recovery
Less discomfort and pain than more invasive procedures
No need for general anesthesia
Decreased risk of infection
No change in eyeglasses prescription (which can occur with scleral buckle procedure)
No double vision
Lower cost
Why do I need pneumatic retinopexy?
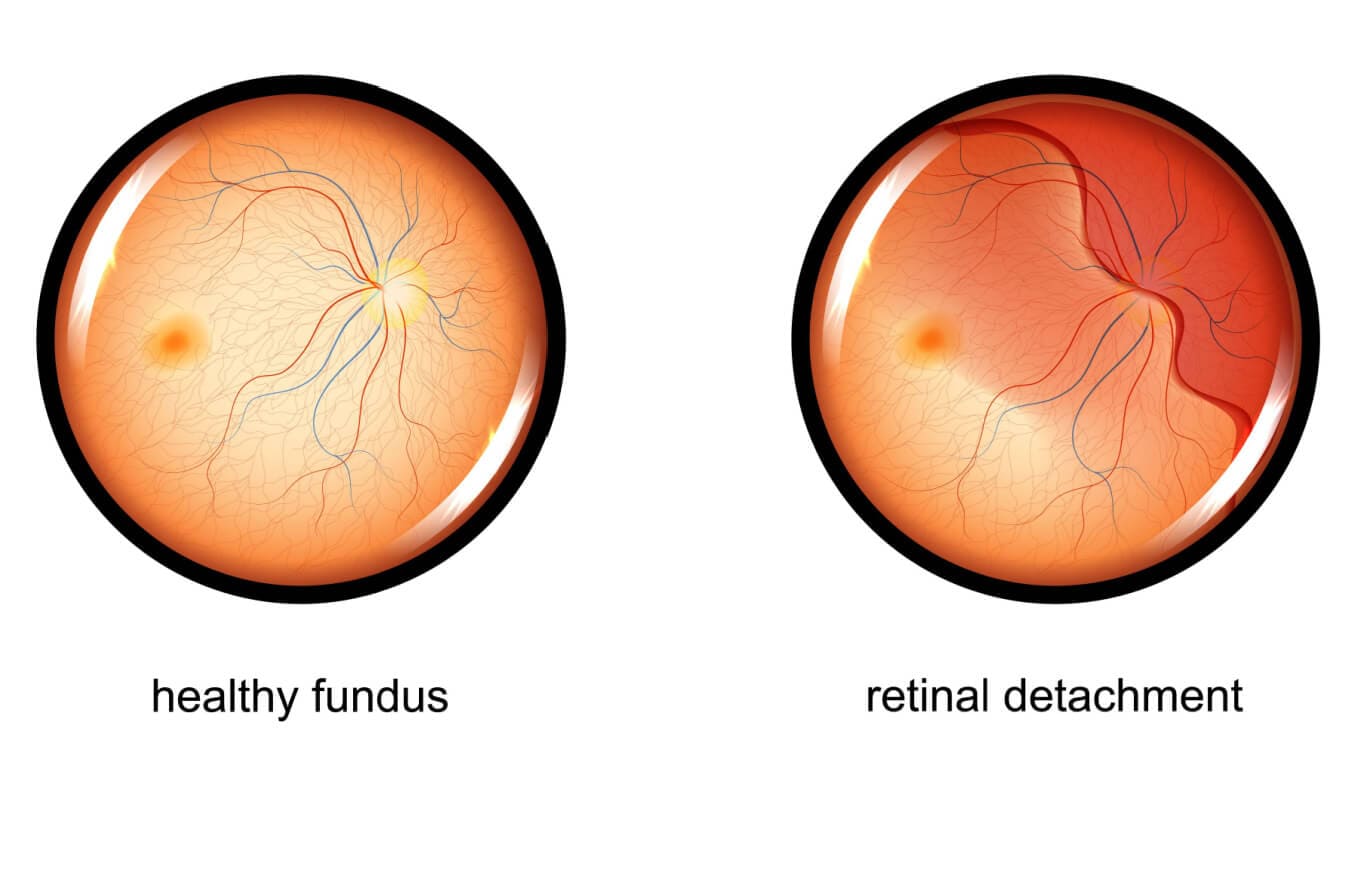
A pneumatic retinopexy is necessary to restore vision that may be lost due to rhegmatogenous retinal detachment. This is the most common type of detached retina. It occurs when a tear or hole in the retina permits fluid from the center of the eye, called vitreous humor, to leak underneath the retina.
The retina is located at the back of the eye. It is a thin tissue that contains specialized nerve cells that turn light entering the eye into signals that are sent to the brain. When the retina peels away from the nourishing tissue underneath — called the choroid — it does not receive the oxygen and nutrients it needs to function.
The retina’s delicate tissue can become injured, leading to severe vision impairment. This condition is particularly sight-threatening if the damage is in the central retina, responsible for our most detailed vision.
When someone’s retina detaches, the following symptoms can occur:
A dark curtain over their vision
Vision may become very blurry or remain unaffected, depending on the location of the detachment. If a large area of the retina is detached, the pupil may not respond properly to light.
Pneumatic retinopexy is performed to reattach the retina, allowing blood supply (and oxygen and nutrients) to return.
Certain factors can put you at higher risk for a detached retina, especially if you:
Are older
Are male
Have high nearsightedness
Have lattice degeneration
Have had cataract surgery
Have a history of certain eye conditions, such as uveitis
READ MORE: Lattice Degeneration: Risks, Treatment and Symptoms
What can I expect during a pneumatic retinopexy procedure?
You will be awake during the procedure, and you may be given some medicine that will help you relax and feel less anxious. After the procedure, you will need to maintain a specific head posture for the next week (explained further in the Posturing section).
How to prepare for the procedure:
Ensure you have a ride to the surgery center and back home. Arrange for someone to help you for a few days if needed.
Stop taking any medication that you have been told to discontinue before surgery.
Limit your intake of food and liquids as advised by your doctor.
You may be given additional instructions based on your eye and medical history.
What to expect during the procedure:
Your eye doctor will explain the procedure to you and ask if you have any questions.
Your other eye will be covered.
You will be given eye drops to dilate the eye and another drop to numb the eye.
You will be given a local anesthetic injection around your eye.
Your doctor will use a syringe to remove some of the fluid in the eye to decrease your eye pressure.
Your doctor will then inject an air or gas bubble into the eye.
Your doctor will use a specialized instrument called a binocular indirect ophthalmoscope (BIO) to see whether the bubble is positioned correctly.
After the treatment, your doctor may put an antibiotic ointment in the eye to prevent infection. They may also give you topical steroid drops to decrease inflammation.
You may be given a patch to protect the eye.
If you have cryopexy or laser retinopexy on the same day, that procedure will often happen first. Your doctor will use a freezing probe or a laser to seal the area around the retinal break. This may also be done in a different order as a 2-stage process. After the gas bubble has been injected and the fluid under the retina has been reabsorbed, your doctor will follow up a few days later with cryopexy and/or laser retinopexy to help reattach the retina.
The procedure should take an hour or less, depending on which other treatments are also performed.
What is recovery from pneumatic retinopexy like?
Your eye doctor will provide instructions about how to care for your eye when you go home. You may be given a prescription for antibiotic drops. You may feel some soreness in the treated eye. If you feel discomfort, you should be able to take an over-the-counter painkiller such as Tylenol.
You will likely have a follow-up visit the next day to monitor your progress. Recovery takes several weeks, and you may have additional appointments during this period.
The gas or air bubble will stay in the eye for about two to six weeks. Your vision will be blurry, and your field of vision and depth perception will be more limited for several days. Over time, you will notice that the bubble will begin to shrink.
Posturing
The bubble needs to maintain slight pressure against your retina for several days to a week to help it reattach. However, holding your head in the wrong position will allow the air or gas bubble to move away from where it needs to be. You will be given specific instructions on how to position your head to keep the bubble in place.
The specific position and the amount of time you spend in this posture will be determined by your doctor. Your detachment has the highest chance of healing if you follow their instructions closely.
Air travel and other restrictions:
You cannot travel by air until the gas or air bubble in your eye is gone and your doctor has given you permission to fly. Consult your doctor regarding driving restrictions and when you can return to work or resume normal activities. It is very important to follow your doctor’s advice to limit complications from the procedure.
What are the risks and complications of pneumatic retinopexy?
Although pneumatic retinopexy surgery has been safely performed for many years, all procedures carry some risk of complications. All in all, most people who undergo pneumatic retinopexy have few complications.
Your risk of complications is impacted by:
Type, size and location of retinal detachment
Age (older than 65 years increases the risk)
Additional eye issues
Medical conditions
Some of the more common risks include:
Fluid becoming trapped underneath the retina
Gas becoming trapped underneath the retina
A scar developing on or beneath the retina
The retina does not reattach or detaches again
Some of the less common risks include:
Inflammation of the eye
Increased pressure in the eye (intraocular pressure)
Development of folds in your retina
Bleeding within the eye
Detachment of the choroid layer
Development of a new retinal tear
If the retina does not reattach or detaches again, you will likely need to repeat the surgery.
When to contact your doctor:
Your doctor will advise you about follow-up appointments. It is important to go to each of these to ensure your recovery is on track. Symptoms such as slight discomfort, tenderness and mild swelling or redness after pneumatic retinopexy are expected. However, some symptoms are not normal, such as:
The onset of new floaters
Flashes of light
A black curtain coming over your vision
New onset of blurry vision or a change in your field of vision
Worsening pain
Increased inflammation around the eye
Pus or discharge from the eye
These symptoms could indicate a complication and should be reported to your eye doctor or an emergency room immediately.